with a C a s t
300 likes | 557 Vues
Nursing the person. with a C a s t. Home Page. Table of contents. Learning outcomes Plaster or fiberglass cast? Caring for a drying cast Cast complications i. Nursing assessments ii. Nursing actions Teaching materials for persons with a cast Quiz Glossary.

with a C a s t
E N D
Presentation Transcript
Nursing the person with a C a s t
Home Page Table of contents • Learning outcomes • Plaster or fiberglass cast? • Caring for a drying cast • Cast complications • i. Nursing assessments • ii. Nursing actions • Teaching materials for persons with a cast • Quiz • Glossary
Learning Outcomes • 1. Compare & contrast plaster & fiberglass casts • 2. Explain the care required while a plaster cast dries • 3. For each complications associated with a cast describe • i. nursing assessments required to detect • ii. nursing actions to treat the complication • 4. Be familiar with teaching materials available for persons who have a cast
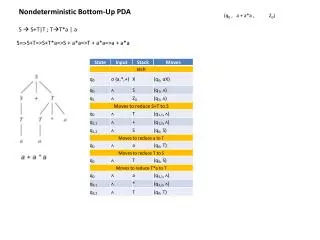
fiberglass casts has durability of plaster but is lighter weight hardens within minutes is porous and there are fewer skin problems does not soften when wet - hair dryer quickly dries skin beneath Costs more plaster casts inexpensive heavy sets in ~ 3 -1 5 minutes, then takes 24 - 72 h to dry (varies with thickness) messy to apply gives more support for ‘bad breaks’
Care required while the plaster cast dries • once applied heat is given off for ~ 15 minutes & may be uncomfortable • while the plaster sets, the cast will remain soft & touching may lead to indentations which may then create pressure spots • until dry handle the cast with palms of hands only - not fingers do not rest cast on hard surfaces or sharp edges
Drying a plaster cast • Picture to be inserted
Presentation on-lineapplication of a fiberglass cast to see click here note the use of 1. Stockinette 2. Padding 3. Casting material
Potential Complications • hidden bleeding • neurovascular compromise • compartment syndrome • skin &/or tissue breakdown • hidden infection from wound &/or ulcer
Bleeding may occur beneath a cast if • there is trauma to the skin at the time of injury • surgery is required to reduce the fracture • this will be documented asORIF • open reduction & internal fixation
To detect bleeding • visualize the cast carefully. Give particular attention to • areas over known wounds &/or incisions • dependent areas - remember that liquid flow follows the line of gravity
Typical appearance (& terminology to describe) • @ 1000 hours Sanguineous Sero-sanguineous @ 1200 hours serous @ 1400 hours
If you see bleeding Mark the outer edges of the bleeding area with time and date & then initial Example: JW Jan 10 - 1000 1200 JW 1400 JW Then ---- >
Follow-up • continue to monitor • instruct client to call you if additional bleeding is noted &/or if s/he notices any other changes • notify MD if • bleeding continues • there is a significant change in vital signs • client condition changes
Document in narrative notes & indicate size location vitals other signs of bleeding Narrative Notes 0845 dark red area ~ 3 cm diameter noted over outer aspect of malleolus; P 88, R 24, BP 108/56; alert but pale; 0930 slight extension of bleeding; client states “feel fine” 1030 no further bleeding noted; P 80 BP 120/ 66 ; instructed to call nurse if further bleeding noted JWladyka RN
Neurovascular Compromise Compression of nerves and blood vessels may be caused by • swelling 2° to injured tissue • impinging bone pieces • swelling 2° to surgery • restrictive pressure 2° the cast
by doing C S M C colour plus • capillary refill (normal < 3 sec) • pulse in affected extremity • [whether present -- no need to count] • temperature of skin S sensation -- do not use a sharp object to assess M able to move extremity & digits
Frequency of C S M • assess q2h X 8, then q4h X 48, then q 8 h • at first sign • elevate limb > heart • give analgesia • if symptoms persist notify MD stat as compartment syndrome may be occurring
If swelling persists • the physician will order the cast to be bivalved • Note - Bivalving may be done by • a physician • an orthopedic technician • a specially trained nurse Burrell et al; 1586
Compartment Syndrome - a special form of neurovascular compromise • muscles, nerves & blood vessels are enclosed in though inelastic fascia (or compartments) • if the muscle within a compartment becomes swollen it cannot stretch & thus the nerves and blood vessels are compressed
Signs & Symptoms • deep, throbbing, unrelenting pain • not controlled by analgesics • often seems out of proportion to the injury • swollen and hard muscle • diminished capillary refill, cyanotic nailbeds, obscured pulse • parasthesia, paralysis
To reverse compartment syndrome A fasciotomy is performed Burrell et al; 1590
Skin &/or tissue breakdown Is most likely if the • cast is resting too close to the tissue -- particularly over boney prominences • cast edges are sharp and irritating the skin
The cast over the area may become warm d/t inflammation beneath if there is skin breakdown there might be drainage if the area becomes infected there may be an odour Diagram to be added Monitor Pressure Areas
Windowing a cast Using cast cutting equipment • an orthopedic tech • MD, or • specially trained nurse cuts out a piece of the plaster over the area of concern if required a dressing is applied Picture to be added
Finishing a cast • If the edges are not covered with stockinette, then you may need to cut small pieces of tape to smooth over the edges -- this is referred to petalling the cast Burrell et al; 1591
Teaching information r/t cast care • Virtual Hospital: Iowa Health Book: Orthopaedics: Instructions for Patients Wearing a Cast
Ready to trythe quiz? I’m ready!
Glossary Capillary refill
References Burrell, Gerlach, Pless. Adult Nursing - Book IX. 2nd ed., Appleton Lang, 1997 Smeltzer, S.C. & B.G. Bare. Brunner & Suddarth’s Textbook of MEDICAL-SURGICAL NURSING. 8 TH ed., Lippincott, 1996. Dykes, P. (1993) Minding the five P’s of neurovascular assessment. AJN, 38 -39. Eden-Kilgour, S. (1993). Understanding neurovascular assessment. Nursing 93. 56-58.