MND
250 likes | 478 Vues
MND. Kate Thomas GPST2 Manorlands Hospice. Outline. MND overview Case study. MND. Selective degeneration of motor neurones Anterior horn cells Motor cranial nuclei Devastating illness Progressive paralysis and eventual death from respiratory failure

MND
E N D
Presentation Transcript
MND Kate Thomas GPST2 Manorlands Hospice
Outline • MND overview • Case study
MND • Selective degeneration of motor neurones • Anterior horn cells • Motor cranial nuclei • Devastating illness • Progressive paralysis and eventual death from respiratory failure • Palliative care involvement from diagnosis
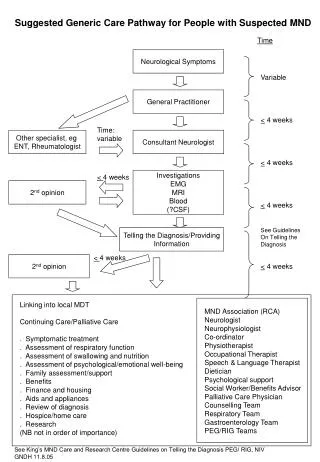
Epidemiology • Incidence 2 per 100,000 • Prevalence 5-7 per 100,000 • 6th and 7th decades • M>F • Sporadic (90%) • Familial MND (10%)
Classifications • Classic MND (65-85%) • Amyotrophic lateral sclerosis (ALS) • Mixed UMN/LMN signs • More rarely • Purely UMN or LMN picture • Primary lateral sclerosis • Progressive muscular atrophy
Bulbar onset • Slurred speech • Wasting and fasciculation tongue • Dysphagia • Association with emotional lability • Respiratory onset • Hypoventilation • Dyspnoea, orthopnoea
Case study • 89 ♂ • AGH (July ‘11) • 3/12 gradual decline, transient left sided weakness, impaired coordination, dysphagia, dysarthria • △△ stroke disease, progressive neurological disorder • CT head: mild invol. change • Rapidly became bedbound, unsafe swallow, incontinent, fasciculations • Dx rapidly progressive MND
At diagnosis • “I’m failing”, “just existing” • Anxiety, fatigue, disturbed sleep • Declined PEG and ventilatory support, accepted NGT • “I don’t want to exist like this” • O/A Manorlands • Apnoeic episodes • Respiratory secretions • Family uncertainty
Communication • 75-80% experience difficulty • Direct effects on muscle control, weakness • Other barriers e.g. Eating, position, distractions
Strategies to improve communication • Time • Place • Mood • Listen • Maintain individuality • Silences, verbal and non-verbal cues • Acknowledge distress • Forward planning
Communication aids • Pen and paper • Pencil grips, book holders, typing sticks/pointers, page turners • MedicAlert bracelet • Signalling systems • Communication boards • Mobile phone • Buzzer • Emergency call alarm
High tech devices • Digitised communication devices • Specific pre-programmed messages • Digitised speech • Specialised phone equipment • Breath-activated hands-free phone, “Type-talk” • Laptop with “text to speech” • Environmental controller • Dedicated speech synthesiser • Eye controlled systems
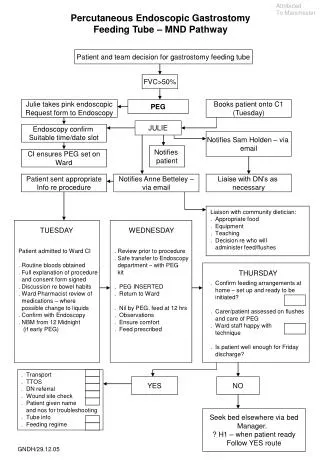
Nutrition and feeding • Malnutrition and weight loss associated with shorter survival • Enteral feeding • When 10% weight loss or BMI <18.5 • Via PEG, RIG or NGT • RIG preferred
Respiratory symptoms • Weakness of ventilatory muscles • Dyspnoea, orthopnoea, hypercapnia • Salivary drooling • Aspiration pneumonia/pneumonitis • Ineffective cough • Anti-cholinergics, postural drainage, chest physiotherapy, suction • Lorazepam, opiates
Ventilation • Alleviate sx of chronic hypoventilation • Improved quality of life • Median survival benefit 7/12 NICE 2010
Anxiety, agitation • Grief reaction to diagnosis • Why me? • How long have I got? • Fears of manner of death • Will it affect my mind? • Will my children be affected? • Often most disabling at night • Environmental factors, reassurance, reversible causes, complementary therapy
Riluzole • Riluzole • 3-4/12m prolongation of life • £3,742 per year Brockington A, Shaw P ACNR 3(5)
Anti-oxidants • Oxidative damage by free radicals implicated in pathogenic process • Cochrane – no evidence for anti-oxidant therapy
Other considerations • Advance directive • Discussion of resuscitation status • Power of attorney • Advocates • PPD • Communication with relatives, carers • Palliative care register
Useful resources • MND Association • MND Scotland