Drugs Affecting the Central Nervous System
850 likes | 1.89k Vues
Drugs Affecting the Central Nervous System. Chapter 5. Central Nervous System CNS. CNS Brain and Spinal Cord Acts as control for regulating physical and mental processes Neurons are the brains functional units. Neurons.

Drugs Affecting the Central Nervous System
E N D
Presentation Transcript
Central Nervous System CNS • CNS • Brain and Spinal Cord • Acts as control for regulating physical and mental processes • Neurons are the brains functional units
Neurons • The brain is a collection of about 10 billion interconnected neurons. Each neuron is a cell that uses biochemical reactions to receive, process and transmit information.
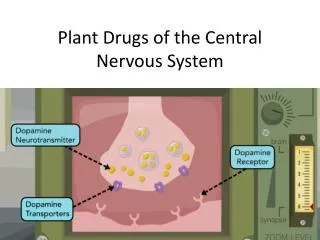
Neurotransmitters • Chemical substances that carry messages from one neuron to another or from a neuron to other body tissues, such as cardiac or skeletal muscles.
Synapses • The synapse is a small gap separating neurons.
Receptors • Proteins embedded in the cell membranes of neurons. • A neurotransmitter must bind to receptors to exert an effect on the next neuron in the chain.
Major Components of CNS • Cerebral Cortex • Thalamus • Hypothalamus
Cerebral Cortex • Involved in all conscious process – learning, memory, reasoning, verbalization, voluntary body movements
Thalamus • Sensation of heat, cold, pain, and muscle position • Relays motor impulses from the cortex to the spinal cord
Hypothalamus • Neuro-endocrine functions • ADH – fluid balance • Body temperature • Regulating arterial blood pressure • Appetite and hunger • Physical changes associated with emotions
Brain • Needs 3 things to properly function • Oxygen – requires more oxygen than any other organ • Glucose – energy source • Thiamine – needed for production and use of glucose
Drugs That Effect CNS • Depressants • Stimulants
CNS Depressants • Mild CNS depressant: decreased interest in surroundings, inability to focus • Moderate CNS depressant: drowsiness or sleep, decreased perception of heat or cold • Severe CNS depressant: unconsciousness or coma, loss of reflexes, respiratory failure and death
CNS Stimulation • Mild stimulation = wakefulness, mental alertness, and decreased fatigue • Moderate stimulation = hyperactivity, excessive talking, nervousness, and insomnia • Excessive stimulation: confusion, seizures, cardiac dysrhythmias
Pain • Pain occurs when tissue damage activates free nerve endings of peripheral nerves • Nociceptors are located in skin, soft tissue, muscle fascia, joint surfaces, arterial walls and periosteum
Opioid Analgesics Opioid analgesics relieve moderate to severe pain in both the central and peripheral nerves.
How do they work? • Decrease pain sensation in brain • Produces sedation • Decreases emotional upset associated with pain • Inhibits production of pain inflammation by prostaglandins
Opioids How given: • by mouth – need high dosages due to first pass through liver • Intramuscular • Intravenous
Opioids Effect on Body • CNS depressant - drowsiness to sleep to unconsciousness to coma • Respiratory – can cause severe respiratory depression • Gastrointestinal: slows gastric motility – constipation
Caution • Patient with • Respiratory depression • Chronic lung disease • Liver / kidney disease • Allergy to drug
Schedule II Drugs • Classification – Opioid analgesics • Morphine • Codeine – often used in combination with acetaminophen – Tylenol with codeine • Hydrocodone – Vicodin - used in combination with acetaminophen / aspirin / ibuprofen • Hydromorphine – Dilaudid - More potent than morphine • Meperidine – Demerol • Oxycodone – Percocet (with acetaminophen) or Percodan (with aspirin)
Morphine Sulfate • Therapeutic classification: opioid analgesic • Pharmacology classification: Opioid agonist • Indications: severe pain (postoperative, fractures, burns) pulmonary edema, and pain associated with myocardial infarct (MI)
Morphine • Action: Binds to opiate receptors in the CNS. Alters the perception of and response to painful stimuli while producing generalized CNS depression Therapeutic Effects: decrease in severity of pain • Adverse Reactions: severe respiratory depression, constipation
Morphine Side Effects • IV maximal analgesia and respiratory depression would occur within 10 to 20 minutes • IM: within 30 minutes • Sub Q: 60 to 90 minutes • PO: peak activity occurs in about 60 minutes * higher dosage needed to metabolism of drug in the liver
Morphine Dosing • Tablets come in 15 mg, 15 mg or 30 mg • Solution for IM, IV or sub Q: 10 mg/ml most common
Nursing Responsibilities • Pain assessment – use appropriate tools • Base-line vitals • Re-asses vitals after pain med administered • Assess bowel function • Overdose: Narcan used to reverse respiratory depression
Pain Scales • Numeric 1-10 • FACES
Assessment • Pain is a subjective experience (whatever a patient says it is) and there are a wide variety of responses to pain. • Culture may effect a persons response • Anxiety or depression can increase ones perception of pain • Fatigue, anger and fear tend to increase pain • Change in vital sign are not always accurate indicators of a patients pain
Evaluation of Effectiveness • Decrease in severity of pain without a significant alteration in level of consciousness or respiratory status. • JCAHO standards dictate that a nurse will evaluate the patients response to the pain medication within 30 minutes to one hour after administration of the pain medication.
Codeine • Therapeutic Classification: allergy, cold and cough remedies, antitussives, opioid analgesics • Pharm classification: opioid agonist • Schedule II drug
Codeine • Action: Binds to opiate receptors in the CNS. Alters the perception of and response to painful stimuli while producing generalized CNS depression – decreases cough reflex – decreases GI motility
Codeine • Side Effects: confusion, sedation, hypotension, constipation • Nursing responsibilities - same as morphine • Evaluation of effectiveness: • Decrease in severity of pain without significant alteration in level of consciousness • Suppression of cough • Control of diarrhea
Codeine • Therapeutic Effects: • Decrease severity of pain • Suppression of a cough reflex • Relief of diarrhea
Codeine Dosing • Usually supplied in combination with other analgesics • Tylenol with codeine • Tylenol # 2 = 15 mg codeine • Tylenol # 3 = 30 mg codeine • Tylenol # 4 = 60 mg codeine • Most often given po with food
Meperidine • Demerol is a synthetic drug with the same uses and adverse effects as morphine • Less nausea and vomiting • Use with caution due to neurotoxic metabolism with chronic use – CNS agitation and confusion, hallucinations, seizures and tremors
Meperidine Dosing • IV or IM • Provided as 10 mg/mL, 50 mg /mL, 75 mg/mL or 100 mg/mL • Dosage for adults: 50 to 150 mg every 3-4 hours • Dosage for pediatrics: 1 to 1.8 mg / kg q 3-4 hours (not to exceed 100 mg dose)
Opioid Antagonists • Block or reverse analgesia, CNS, respiratory depression • Competes with opioids for opioid receptor sites in the brain and prevents opioid binding with receptors or displaces opioids that have already occupied the receptor sites.
Naloxone or Narcan • Naloxone is the oldest and has long been the drug of choice to treat respiratory depression caused by an opioid drug. • IV, IM or Sub Q acts in minutes and last for 1 to 2 hours
Use in Special Populations • Opiate tolerant clients • Pediatric patients • Geriatric population • Renal and hepatic impairment • Critical Care • Cancer
Chapter 7 Analgesic – Antipyretic – Anti-inflammatory
Prostaglandins • Chemical mediators found in most body tissue – they help regulate many cell functions and participate in the inflammatory response
Pain – Fever - Inflammation • Pain can occur with injury or tissue inflammation • Fever is elevation of body temperature above the normal range. • Inflammation is the normal body response to tissue damage – it is the attempt by the body to remove the damaging agent and repair the damaged tissue.
Mechanism of Action • Aspirin and other NSAIDs inhibit prostaglandin synthesis in the central nervous system and the periphery. • Acetaminophen action on prostaglandin is limited to the central nervous system – less effective in reducing inflammation. • Both inhibit cox enzymes which are required for prostaglandin formation
Indications for Use • Aspirin, NSAIDs and acetaminophen are used to prevent and treat mild to moderate pain and or inflammation associated with musculoskeletal disorders, headache, menstrual cramps, minor trauma, or minor surgery
Aspirin • Usage has declined since new NSAIDs developed. • Cause GI upset – GI bleeding • Low dosage ASA used as preventive measure against stroke or myocardial infarction • Contraindicated in children due to Ryes Syndrome
Acetaminophen • Commonly used as an aspirin substitute for fever and pain but lacks the anti-inflammatory and anti-platelet effects.
Tylenol Most Common Brand • Action: inhibits the synthesis of prostaglandins that may serve as mediators of pain and fever, primarily in the CNS. Has no significant anti-inflammatory properties or GI toxicity. • Metabolism: 85-98% by the liver – may be toxic in overdose situation – excreted by kidneys.
Drug-drug interaction • Chronic high dose acetaminophen (greater than 2 gram per day) may increase the risk of bleeding with Warfarin (Coumadin) • PT should be monitored and INR not to exceed 4 • Hepatotoxic with other hepatotoxic substances including alcohol. • Combines use with NSAIDs increased risk of adverse renal effects. • May decrease effects of loop diuretics - Lasix