MAM Decision-making Tool
410 likes | 900 Vues
MAM Decision-making Tool. Meeting Objectives. Review the MAM decision-making tool Work through country situation Provide feedback on Content Usability Layout. Moderate Acute Malnutrition (MAM). Background Review of supplementary feeding programs (2007)

MAM Decision-making Tool
E N D
Presentation Transcript
Meeting Objectives • Review the MAM decision-making tool • Work through country situation • Provide feedback on • Content • Usability • Layout
Moderate Acute Malnutrition (MAM) Background • Review of supplementary feeding programs (2007) • WHO consultations MMI (2008) and MMII (2010) • Dietary needs • Programme approaches to manage MAM • NUGAG review on MAM • Limited guidance on programming • Differing approaches • Increase in products available for programming CONFUSION!!!
Moderate Acute Malnutrition (MAM) • Burden of MAM • 11 million children affected globally • 41 million children • 3 x risk of death compared to well-nourished • Increased risk of acute malnutrition in emergencies
MAM Taskforce Additional Members WHO ECHO • Formed by the Global Nutrition Cluster • UNHCR • UNICEF • WFP • OFDA • ACF • Save the Children • CDC
Tool Objectives Decision making process grounded by data, but is subjective on some levels • Guide practitioners to identify most appropriate and feasible strategies to address MAM • Prevention • Management (treatment) • Harmonize nutrition programme decision-making on MAM in emergency situations • Incorporate contextual situational factors into the decision making process • Beyond nutritional status • Engage in discussion
Caveats of Tool • Limited to emergency contexts • Rapid/sudden onset • Slow onset • Protracted emergencies • Acute emergency within a chronic emergency setting • Local or large-scale emergencies • Not for refugee contexts • UNHCR/WFP Guidelines for Selective Feeding: The Management of Malnutrition in Emergencies 2011 http://www.unhcr.org/4b7421fd20.pdf
Caveats of Tool • Primary objective: prevent morbidity and mortality associated with MAM • Linkages: MAM cannot be addressed in isolation • SAM • IYCF-E • Other sectors (WASH, health, food security) • Re-assessment
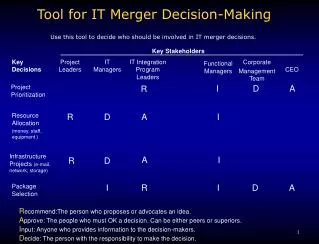
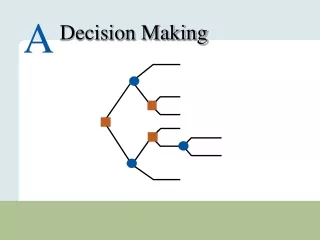
MAM decision tool steps Prevention/treatment Prevention Treatment No additional programme Step 1: Programme Type/Objective Step 2: Modality Supplementary feeding Cash/voucher Infant and Young Child Feeding Target group Product Duration Delivery Step 3: Programme Operation Step 4: Review and Revise Regularly throughout the emergency
Data Needs • Prevalence of GAM in the affected area (current or historical) • Information nature and severity of the crisis (risk) • Baseline health data in affected areas • Expected impact on morbidity • Food security situation • Expected impact on food security • Population data • Displacement • Density
Nutritional Data MAG scenarios for the tool • High >15% • Medium 8-15% • Low <8% Sources • Trend data • Seasonality • Admission data (coverage should be assessed) • Screening data
Morbidity • Malnutrition Infection Cycle • Likelihood of morbidity and/or outbreak to impact GAM • Baseline data • Vaccination coverage, vitamin A coverage, disease profile • WASH services • Access to care
Food Security Magnitude, extent, severity and duration of the crisis on food security Household consumption and market data sources
Displacement • Influences type and frequency of programme • Many different contexts and types of displacement • Dispersed settlements, mass shelter in collective centers, reception and transit camps, self settled camps, planned camps (official and unofficial), IDPs with host populations
Population Density • Risk of morbidity • Consider in programme delivery design • Example: low GAM, but high density= large number of children in need • Haiti, post earthquake in Port au Prince • Kenya, post election violence in urban centers
MAM decision tool steps Prevention/treatment Prevention Treatment No additional programme Step 1: Programme Type/Objective Step 2: Modality Supplementary feeding Cash/voucher Infant and Young Child Feeding Target group Product Duration Delivery Step 3: Programme Operation Step 4: Review and Revise Regularly throughout the emergency
Prevention: Modality Infant & Young Child Feeding in Emergencies Component IYCF-E support Blanket Supplementary Feeding • Provision of supplementary food • Platform for other interventions • Screenings + referrals • Child survival (deworming, vit A, immunisation) • Health/nutrition education Cash or Voucher • Cash/voucher if food and nutrient availability is good, markets functioning, caring practices maintained • Further research needed • Specialised product + cash • Cash 4X value of specialised product
Prevention: Target Group BSFP should not be expanded to beyond 6-59 months and PLW except under serious conditions The general food distribution (GFD) should meet the needs of other household members. Advocacy for improving the GFD or other food security measures. • Children under 5 at increased risk mortality • Target children 6-59 months • If logistical constraints consider reducing target group • PLW • No standard criteria for enrollment • Impact on IYCF-E • MAM treatment programming exist • Low birth weight • Prioritise • children over PLW • lactating over pregnant women (protecting 0-6 month old infants)
Prevention: Product Considerations • Government approval • Objective of the intervention & target group • Some products are targeted for 6-23/36 months • Household’s ability to cook • Are there cooking facilities, easy access to fuel and water? • Cultural practices and food preferences • Corn, wheat & rice based supercereals • RUFs- peanut, chickpea and milk based (limited quantities) • Nutrient gap (energy & micronutrient) • Decide upon higher or lower level energy • HH food security, diet diversity, baseline diets, chronic malnutrition, micronutrient deficiencies • Sharing practices, household use of foods, access to other foods
Recommended Products and Alternatives ± Only where supplement is the primary source of available food
Prevention: Duration and Exit Strategy • Duration of BSFP based on scale & severity of emergency • GAM + Risk of deterioration • Generally 3-6 months • Example start at least 1 month prior to leans season and run until post-harvest • Regular re-assessment • Scaling up or down • Extension • Rolling admission and no discharge (exiting) until end of programme (even if child is older than upper limit at the close of programme)
Prevention: Delivery Mechanism Considerations • Access to the population • Security, seasonal, physical • Scale of crisis (total area affected) • Implementation capacity • Low or security- consider combining with GFD • Population density • Determine number of sites • If dense, may need multiple days/week for distribution
Prevention: Delivery Mechanism BSFP stand alone programme • Targeted directly to households with children BSFP Integrated delivery • Child’s supplementary food is added to food/cash/voucher distribution • Low security context • Rapid onset immediate programming • Exclusion and inclusion errors • Shift to parallel independent programme as soon as feasible
Treatment • Targeted Supplementary Feeding (TSFP) • Treatment for MAM with nutritious food supplement and routine medical care • Admission/discharge criteria based on anthropometric measures (national or international guidelines) • Nutrition communication • Support for IYCF-E Cash/vouchers need more evidence
Treatment: Target Group Malnourished children 6-59 months Discharges from SAM Pregnant and lactating (up to 6 months postpartum) women Chronic illness (HIV, TB) Exceptions Infants <6 months not admitted, support IYCF strengthened Other vulnerable populations identified (disabled children , 5-10 years olds, older people)
Treatment: Product Considerations • Government approval • Target group • Household’s ability to cook • Are there cooking facilities, easy access to fuel and water? • Cultural practices and food preferences • Corn, wheat & rice based supercereals • RUFs- peanut, chickpea and milk based (limited quantities)
Recommended Products and Alternatives ± Only where supplement is the primary source of available food
Treatment: Duration and Exit Strategy • Treatment range 1-4 months • Scale down of TSFP considered when: • GAM <5% • No aggravating factors • Low numbers of admissions in MAM and SAM treatment may also be used to decide to phase out • Be mindful of programme coverage and performance
Treatment: Delivery Mechanism Considerations • Access to the population • Security, seasonal, physical • Scale of crisis (total area affected) • Implementation capacity • Low or security- consider combining with GFD • Population density • Determine number of sites • If dense, may need multiple days/week for distribution
Treatment: Delivery Mechanism • Linked closely to treatment of SAM under CMAM model • TSFP sites adjacent to OTP or health centres support referrals (both directions) • Large area for distribution/services • If mobile or away from health centres provide basic health interventions • Considerations • Health service coverage, existing MAM/SAM programmes, capacity to scale-up
Prevention &Treatment • Both prevention and treatment may be recommended • Follow the previous steps to design each programme • Think through linkages between programmes • Ideally, children should not be simultaneously enrolled in both programmes • In reality, the risks associated with non-participation outweigh the cost of dual participation • In some large emergencies children should be enrolled in prevention programmes as they may come in and out of treatment • Example: Northern Kenya, 2011/12
No Additional Intervention Emergency programming is in addition to existing nutrition programmes • Additional programs not needed • Existing nutritional programs • Re-evaluate risk as emergency progresses • Build into nutrition response plan • Strengthen support for IYCF or micronutrient programmes
MAM decision tool steps Prevention/treatment Prevention Treatment No additional programme Step 1: Programme Type/Objective Step 2: Modality Supplementary feeding Cash/voucher Infant and Young Child Feeding Target group Product Duration Delivery Step 3: Programme Operation Step 4: Review and Revise Regularly throughout the emergency
Programme Linkages Interventions in emergencies: Addressing acute malnutrition Selective feeding programmes General Food Distribution IYCF-E MAM Programmes Treatment for SAM Addressing underlying causes of undernutrition Prevention Blanket feeding Cash/voucher Outpatient treatment WASH Food security Health Treatment Targeted Inpatient treatment Addressing micronutrient deficiencies
Additional Feedback • Josephine Ippe: Global Nutrition Cluster jippe@unicef.org • Lynnda Kiess: World Food Programme lynnda.kiess@wfp.org My contact: Leisel Talley, Centers for Disease Control and Prevention: Ltalley@cdc.gov