History
930 likes | 1.23k Vues
History. 12 yo boy A month ago he had an upper resp infection Now presents with 3 week history of fatigue, easy bruising and nose bleeds Physical exam is normal except for a few scattered bruises on his legs. Labs. WBC: 2500 (normal 4000-10,000) HCT: 25 Normal MCV Platelets: 12,0000

History
E N D
Presentation Transcript
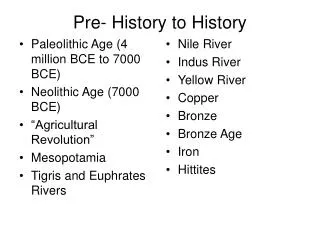
History • 12 yo boy • A month ago he had an upper resp infection • Now presents with 3 week history of fatigue, easy bruising and nose bleeds • Physical exam is normal except for a few scattered bruises on his legs
Labs • WBC: 2500 (normal 4000-10,000) • HCT: 25 Normal MCV • Platelets: 12,0000 • Reticulocyte count: 12,000 (normal 40-90,000) • LDH: normal
Questions • What is the diagnosis? • What treatment options might you offer? • What is the suspected etiology? • Did leukemia enter your differential? How did you rule it out?
History • 12 year old boy • Presents with 4 week history of fatigue, easy bruising, nose bleeds and low grade fever • On physical exam he appears ill, listless
Labs • WBC 2500 • HCT: 25 • PLAT: 12,000
Questions • What is the diagnosis? • What are common treatment options? • What additional sites (besides the bone marrow) do you need to be concerned about?
History • 75 yo woman presents with fatigue and diffuse joint pain for several years but worse recently • Physical exam reveals a chronically ill appearing woman. Joints appear swollen and stiff.
Labs • WBC 5,000 • HCT: 29.5 • MCV: 78 (normal 82-95) • Platelets: 508,000 (normal 150-400,000) • ESR: 30 (normal < 20) • Total protein elevated
Questions • What is her protein problem? • What more information would you like?
More labs • Iron: 20 (normal 30-160) • TIBC: 200 (normal 250-350) • % saturation 30% (normal 20-50) • Ferritin: 100 (normal 11-300)
Questions • What is the diagnosis? • What are you going to do about it?
More history • You diagnosed rheumatoid arthritis and started her on prednisone • Initially she seemed a lot better with less joint pain and more mobility • A year later she is feeling much more fatigued and has shortness of breath walking across the room
Labs • WBC: 5000 • HCT: 23 • MCV: 72 • Platelets: 600,000
More labs • Iron: 10 • TIBC: 350 • % saturation 4 % • Ferritin: 20
Questions • What happened to this patient’s blood count • What are some possible diagnoses • What further workup are you going to do? • How would you treat this patient?
HISTORY • 75 yo man who presents with severe back pain, nausea and vomiting, and a lot of fatigue over the past few months • Labs: • WBC: 4000 • HCT: 23.5 HGB: 7.8 • BUN 80 Creatinine 4.0
Additional work up • Immunoelectrophoresis • Ig G kappa • Quantitative immunoglobins • Ig G: 5000 mg/dl • Ig A: 20 mg/dl • Ig M: 15 mg/dl
Questions • What stage is this person? • What treatments might you think about?
History • 70 yo man comes in complaining of 6 month history of progressive fatigue • Has trouble concentrating • Notes some shortness of breath with exertion • On exam: distended neck veins, retinal hemorrhages, appears plethoric • Has a palpable spleen tip
Labs • WBC: 3000 • HCT: 34 • MCV: normal • Platelets: 110,000 • Total protein 10 (normal 6-8)
Immunoglobulins • Ig G: 200 (normal 600-1600) • Ig A: 40 (normal 73-347) • Ig M: 3500 (normal 46-300)
Questions • Would you expect: • Anemia? • Lytic bone lesions? • Lymphadenopathy • Hypercalcemia? • Hepatosplenomegaly • What complication does this patient have? • What would you do about it?
History • 70 yo man comes in complaining of 6 month history of progressive fatigue • Has trouble concentrating • Notes some shortness of breath with exertion • On exam: distended neck veins, retinal hemorrhages, appears plethoric • Has a palpable spleen tip
Labs • WBC: 16,000 (normal 5000-10,000) • HCT: 60 • MCV: 75 (normal 85-95) • Platelets: 550,000 (normal 150-450,000)
What is your differential?How would you rule each possibility out? • Hypoxia/lung disease • Tumors excreting erythropoietin • Smoker’s polycythemia • Spurious polycythemia
Questions • What is the therapy for this condition? • What potential long term outcomes can occur? • What special instructions would you give this patient? • What other symptoms might you ask about?
History • A healthy 22 year old woman comes into your clinic feeling well but complaining of a rash over the past week.
LABS • WBC: 8,000 • HCT: 37 • Platelets: 10,000
Questions • What is the diagnosis? • Did you need the bone marrow to make it? • What are potential causes of this condition? • What are the common treatments used?
History • 33 yo man comes in with a 2 month history of tightness in his chest and some shortness of breath and a dry cough • On questioning he admits to a 15 pound weight loss and feeling hot and sweaty at night • Exam reveals some rubbery non-tender nodes in his right axilla and supraclavicular area
Questions • What is your differential diagnosis? • What would you do next? • What other labs might you think about?
Pathology • Diffuse infiltration with large lymphoid cells which are CD 20 positive
Questions • What stage is he? • What therapy would you offer him? • What can you tell him about his prognosis?