Diarrhea
340 likes | 965 Vues
Diarrhea. A messy subject. Case. A 1 year old girl is brought to clinic with 3 days of watery brown diarrhea, vomiting, and irritability. On exam the child is lethargic, afebrile, with sunken eyes and a weak pulse of 140/minute. Which of the following is the best management plan?

Diarrhea
E N D
Presentation Transcript
Diarrhea A messy subject
Case A 1 year old girl is brought to clinic with 3 days of watery brown diarrhea, vomiting, and irritability. On exam the child is lethargic, afebrile, with sunken eyes and a weak pulse of 140/minute. Which of the following is the best management plan? • Check CBC and stool tests for pathogens • Prescribe oral rehydration solution • Prescribe oral antibiotics • Begin IV fluids and hospitalize
Please make your selection... • Choice One • Choice Two • Choice Three • Choice Four
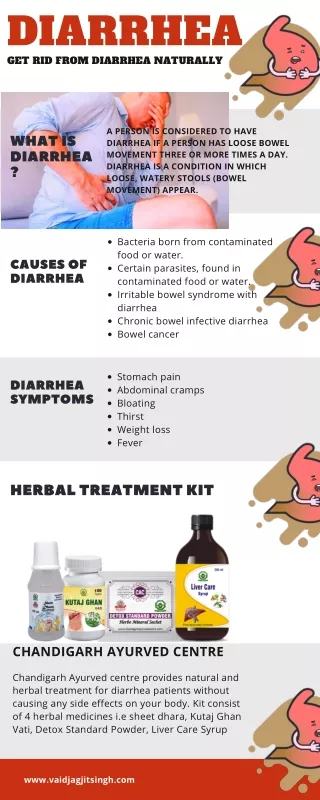
“More than 70 per cent of almost 11 million child deaths every year are attributable to six causes: diarrhoea, malaria, neonatal infection, pneumonia, preterm delivery, or lack of oxygen at birth.” - UNICEF
Deaths per year from diarrheal illness • United States: 6,000 • Developing world: 1.5 to 2 million (children < 5 years old) World Gastroenterology Organization (WGO) Practice Guideline Acute Diarrhea (March 2008)
Classification WGO Practice Guideline – Acute Diarrhea March 2008
Acute diarrhea: clinical priorities • Assess severity of illness and need for rehydration • Identify likely causes on the basis of history and exam
Exam: volume status • Adults and Children • Tachycardia, postural hypotension • Jugular venous distension • Mucous membranes • Children • Urine output, Dry mouth/eyes • Sunken fontanelle • Skin turgor • Irritable or lethargic, Drinking poorly
Kwashiorkor: lack of protein Marasmus: protein + calorie malnutrition www.cs.stedwards.edu www.glahaiti.org Malnutrition is a major risk factor for diarrhea mortality
History suggests etiology • Fever, bloody stool, tenesmus • Inflammation • Invasive and cytotoxin producing pathogens • Profuse watery stool • Secretory diarrhea • Cholera, viral pathogens, Giardia • Vomiting • Viral pathogens, ingested bacterial toxins
Lab tests • Stool for ova and parasites • Especially in severe or chronic diarrhea • Fecal leukocytes • Suggests colitis, invasive organism • CBC and electrolytes • Won’t alter acute Rx, unless there are signs of severe anemia • Stool culture • Often not available or required • Stool Sudan stain (fecal fat) • In chronic diarrhea with weight loss
Oral rehydration saves lives WGO Practice Guideline – Acute Diarrhea March 2008
Oral rehydration solution (ORS) Rice-based ORS is superior to glucose-based ORS in patients with cholera WGO Practice Guideline – Acute Diarrhea March 2008
Rehydration of children WGO Practice Guideline – Acute Diarrhea March 2008
Rehydration of children WGO Practice Guideline – Acute Diarrhea March 2008
Medical therapy - children • Admit to hospital if malnourished, severely dehydrated, age < 1 year, recent measles • ORS if dehydrated; IV fluids (RL, NS) if severely dehydrated; rehydrate over 3 to 6 hours • Re-feed as soon as rehydration is accomplished • Zinc 20 mg daily x 14 days • Antibiotics not usually indicated • Give antibx for: • Dysentery • Suspicion of cholera • Giardiasis or amebiasis
Medical therapy - adults • ORS or IV fluids (RL, NS) if severely dehydrated • Bismuth or loperamide (contraindicated if there is fever or bloody stool) • Antibiotics not usually indicated • Give antibx for: • Dysentery (some cases) • Suspicion of cholera • Giardiasis or amebiasis
Dysentery • Bloody stools • Shigella, enterohemorrhagic E coli (EHEC), other bacteria – often with fever • Amebiasis – no fever (unless in liver) • Antibiotics recommended for extremes of age, immunocompromised or malnourished patients, suspicion of sepsis or enteric fever • Antibiotic Rx may precipitate hemolytic-uremic syndrome in children, especially in industrialized countries
Bacteria resistance is common – learn local patterns WGO Practice Guideline – Acute Diarrhea March 2008
Chronic diarrhea - children • Among infants in developing countries, 20% of acute diarrheal illnesses become chronic • Enteropathogenic E coli (EPEC), Giardia • Vicious cycle of diarrhea and malabsorption leading to death • Consider HIV • Rx is largely nutritional: • Iso-osmolar carbohydrate porridge, via feeding tube if needed • MVI and zinc • Antibiotics for EPEC, Giardia
Chronic diarrheal syndromes - adults • Campylobacter ileitis: chronic diarrhea, signs of inflammation • Giardia, ameoba • Wasting? Consider HIV, TB • Fat in stool? Consider sprue, chronic pancreatitis
CaseA 1 year old girl is brought to clinic with 3 days of watery brown diarrhea, vomiting, and irritability. On exam the child is lethargic, afebrile, with sunken eyes and a weak pulse of 140/minute. Which of the following is the best management plan? • Check CBC and stool tests for pathogens • Prescribe oral rehydration solution • Prescribe oral antibiotics • Begin IV fluids and hospitalize
Resources WGO Practice Guideline – Acute Diarrhea March 2008