Symptomatic epilepsy – identifiable cerebral cause.
130 likes | 496 Vues
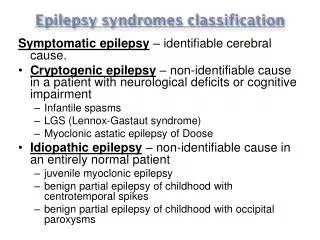
Symptomatic epilepsy – identifiable cerebral cause. Cryptogenic epilepsy – non-identifiable cause in a patient with neurological deficits or cognitive impairment Infantile spasms LGS (Lennox-Gastaut syndrome) Myoclonic astatic epilepsy of Doose

Symptomatic epilepsy – identifiable cerebral cause.
E N D
Presentation Transcript
Symptomatic epilepsy – identifiable cerebral cause. • Cryptogenic epilepsy – non-identifiable cause in a patient with neurological deficits or cognitive impairment • Infantile spasms • LGS (Lennox-Gastaut syndrome) • Myoclonic astatic epilepsy of Doose • Idiopathic epilepsy – non-identifiable cause in an entirely normal patient • juvenile myoclonic epilepsy • benign partial epilepsy of childhood with centrotemporal spikes • benign partial epilepsy of childhood with occipital paroxysms
Important Epilepsy Syndromes: • West syndrome – Triad of: • hypsarrhythmia on EEG • infantile spasms • developmental retardation or regression • Presents in 6-18 month infants and is treated with ACTH or vigabatrin. • Lennox-Gastaut Syndrome (LGS) – Infantile spasms and West syndrome frequently transform into LGS becoming a life-long epileptic encephalopathy. It consists of: • atonic seizures • tonic seizures • atypical absence seizures associated with mental retardation and a characteristic EEG pattern. • Typical onset of LGS is between 3-5 years of age. EEG shows an abnormally slow background and diffuse slow spike and slow wave (<2.5 Hz) activity due to generalized encephalopathy. • Childhood Absence Epilepsy – occurs between 3-5 years of age and remits by ages 10-12 years. Frontally dominant EEG showing normal background for age and 3-Hz generalized spike and wave discharges. Usually 4 Hz at the onset of the absence seizures and may slow to 2.5 Hz at the end of a seizure. • Benign partial epilepsy syndromes of childhood – there are two important types: • Benign rolandic epilepsy (BRE) or Benign partial epilepsy of childhood with centrotemporal spikes – onset is between 3-10 years with history of orobuccal numbness on one side of the mouth or with a tingling sensation on one side of the face. EEG shows frequent spike and wave discharges in the centrotemporal region. • Benign partial epilepsy of childhood with occipital paroxysms (BPEOP) – similar to BRE but the discharges are located in the occipital part of brain. • Juvenile Myoclonic Epilepsy (JME)- the most common epilepsy syndrome presenting with generalized tonic-clonic seizures in an other-wise neurologically normally patient aged 12-30 years. Photosensitivity is present in at least 30% of patients. • Clue words for the boards: • slow spike and wave activity = LGS • diffuse 3-Hz spike and wave activity = benign absence epilepsy • fast spike and wave (>2.5 Hz) activity = benign myoclonic types of epilepsy • hyperarrhythmia = infantile spasms
Syncope; Transient ischaemic attack (TIA); Transient global amnesia; Panic attack; Episodic vertigo; Stroke; Migraine; Memory disturbance and/or confusion; and Restless legs syndrome
50% of patients Depression, Anxiety and Psychotic disturbances These psychiatric disturbances can be classified according to how they relate in time to seizure occurrence, ictal periictal(preictal/prodromal, postictal) interictal.
Treatmentrelated psychiatric problems Antiepileptic drugs most commonly depression, anxiety, behavioural or cognitive problems and, in rare cases, psychosis. Phenobarbitone, primidone, tiagabine, topiramate, vigabatrin and felbamate have been associated with depression. Psychosis is a rare complication of a number of AEDs such as vigabatrin and topiramate. Improved seizure control has been associated with the emergence of psychiatric symptoms. Landolt introduced the term ‘forced normalisation’ which refers to a dramatic reduction in epileptiform activity on EEG being associated with the emergence of psychosis or sometimes behavioural/mood disturbances. This phenomenon has been reported with most AEDs and therefore any new drug should be started at low doses and increased slowly. The risk may be higher in patients who are on polytherapy, become seizure free abruptly, or if there is a past psychiatric history.
Epilepsy surgery Transient mood disturbances (emotional lability, depression and anxiety) have been reported following temporal lobe surgery for epilepsy (about 25%) in the first 6-12 weeks. in some patients (10%), symptoms, particularly depression, may persist and require psychiatric treatment. There are also reports of de novo psychosis arising after surgery and it has been suggested that it is more common with right sided temporal lobe surgery. It is therefore important for pre and postsurgical psychiatric evaluation to form part of the assessment/management for epilepsy surgery.
MAGNETIC RESONANCE IMAGING (MRI): Each patient with new-onset epilepsy should have an MRI (temporal angulation, T1,T2, FLAIR, coronal and axial) to detect structural lesions caused by for example cortical malformation, traumatic brain injury, brain tumor, and cerebrovascular disease, which are the most common causes of symptomatic epilepsy. Contrast media, inversion recovery, fast field echo and 3D only in special cases. Even in idiopathic epilepsy, MRI is recommended to diagnose unsuspected dual pathology as discussed above. ELECTROENCEPHALOGRAM (EEG): Each patient with newonset epilepsy should have an EEG. EEG is most valuable within 24 h of the seizure. Information gain is optimal up to the 4th EEG, if no paroxysmal interictal discharges are found, repeat EEG during sleep. 24-hour EEG most meaningful in a patient with frequent seizures who can be expected to have seizures during the 24 h recording. Interictal EEG discharges may support the diagnosis of the epilepsy syndrome. COMPUTER TOMOGRAM (CCT): Computer tomograms are obsolete, except to detect fractures or hemorrhage in an emergency situation. HEAD X-RAY: obsolete CLINICAL CHEMISTRY: routine work-up, creatinkinase, Vitamin B6 if seizures are unresponsive to AEDs, even in adults. CSF, only when infectious disorders are suspected. Creatinkinase increased within 12-24 h, prolactin increased within 30 min. SINGLE-PHOTON- EMISSION -TOMOGRAM (SPECT) and POSITON- EMISSION-TOMOGRAM (PET), MAGNETO ENCEPHALOGRAPHY (MEG): only for presurgical work-up or scientific studies.
Suggested MRI protocols for epilepsy patients (standard investigations) Temporal lobe epilepsy 1. Hippocampal oriented T2-weighted (coronal + axial) 2. Hippocampal oriented fluid-attenuated inversion recovery (FLAIR) (coronal + axial) 3. Isotropic T1-weighted three-dimensional sequence (MPRage) 4. (Gadolinium contrast-enhanced T1-weighted image if non-contrast-enhanced image is inconclusive) 5. T2*-weighted sequence Extratemporal lobe epilepsy 1. AC–PC oriented T2-weighted (coronal + axial) 2. AC–PC oriented FLAIR (coronal + axial) 3. Isotropic T1-weighted three-dimensional sequence (MPRage) 4. (Gadolinium contrast-enhanced T1-weighted image if non-contrast-enhanced image is inconclusive) 5. T2*-weighted sequence Special protocols: Rationale 1. T2 relaxometry hippocampal signal abnormalities 2. Magnetic resonance spectroscopy detection of metabolic abnormalities 3. Diffusion tensor imaging (DTI) investigation of fiber tracts 4. Functional MRI investigation of eloquent cortical areas 5. Three-dimensional sequences automated voxel-based analyses 6. Magnetic resonance angiography investigation of brain vascularization