Why Low-Temperature?
370 likes | 951 Vues
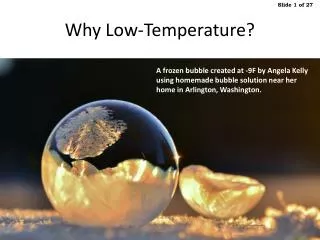
Why Low-Temperature?. A frozen bubble created at -9F by Angela Kelly using homemade bubble solution near her home in Arlington, Washington. Sterilization Methods. FDA 510K – Sterilization Guidance Timeline. Evolution of Submission Process Driven by Technological Innovation.

Why Low-Temperature?
E N D
Presentation Transcript
Why Low-Temperature? A frozen bubble created at -9F by Angela Kelly using homemade bubble solution near her home in Arlington, Washington.
FDA 510K – Sterilization Guidance Timeline Evolution of Submission Process Driven by Technological Innovation Medical Device Amendments to Food, Drug and Cosmetic Act of 1997 *1 Addition of novel non-traditional category When to submit a 510K for a change to an existing device Food, Drug and Cosmetic Act - Section 510K Pre Market Notification Clarification on traditional and non-traditional sterilization methods *1 Clinton, William J. (21 November 1997). "Statement on Signing the Food and Drug Administration Modernization Act of 1997
FDA 2008 - Recommended Review Routing Early Consultation with FDA: Key to QS Inspection Success http://bit.ly/Sterility-Info-for-510k INCB = Infection Control Devices Branch
# Test Name # Cycles # Of Samples Notes Required Optional 1 Residual 2X 5 samples Run with CytoTox test R 2 CytoTox 2X 5 samples Run with residual test R 3 Animal testing 2X 5 samples Only if CytoTox fails O 4 Physical QC 2X 5-10% of load Verify product & packaging functional after 2X sterilization R 5 Accelerated Aging 2X Amount product in one shipping carton Run ASTM “Shake & Bake” test immediately after R 6 ASTM Shake 1X Amount of product in one shipping carton Verify package integrity R 7 % Efficiency of Recovery 1X 5 samples minimum non sterile product Validate extraction method for the Bioburden test method R 8 Product Bioburden 3X 10 samples each lot Run three different lots, non sterile product R 9 Product Bioburden versus BI/PCD 1X 20 samples – 10 TSB / 10- FTM Compare product Bioburden against BI/PCD O 10 PQ Micro per ISO 14937 Full load with packaging - 3 ½ cycles - 1 sublethal cycle - 3 full production runs R 11 BI Titer Perform on every BI lot Initial validation lot, all production lots O Recommended & Required Testing for FDA Submissions
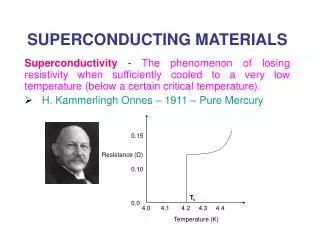
Medical Device Approval Process Identifying the Right Offices within FDA Critical to Success
SAL and Overkill Sterility Assurance Level (SAL) Overkill Cycle • Microbiology term to describe the probability of a single unit being non-sterile after it has been subjected to the sterilization process • SALs can be used to describe the microbial population that was destroyed by the sterilization process. Each log reduction (10−1) represents a 90% reduction in microbial population. • A 10−6 SAL (12-log reduction) will reduce a population from a million organisms (106) to very close to zero, theoretically. 3MTM Attest™ Products Sterile U Network - T U T O R I A L S Living Organisms for Sterility Assurance— Biological Indicators
ISO 14937:2009 http://bit.ly/ISO14937
Other ISO Standards ISO 11737-1: 2006 – Sterilization of medical devices – Microbiological methods – Part 1: Determination of a population of microorganisms on products ISO 11737-2: 2009 – Sterilization of medical devices – Microbiological methods – Part 2: Tests of sterility performed in the definition, validation and maintenance of a sterilization process
Low-Temp Steam & Formaldehyde EN 14180:2003 - Sterilizers for medical purposes. Low temperature steam and formaldehyde sterilizers. Requirements and testing BS EN ISO 25424:2011 - Sterilization of medical devices. Low temperature steam and formaldehyde. Requirements for development, validation and routine control of a sterilization process for medical devices BS EN ISO 11138-5:2006 - Sterilization of health care products. Biological indicatorsBiological indicators for low-temperature steam and formaldehyde sterilization processes
Microbial Load Determination(ISO 11737-1:2006) Packaged Product (non-sterile) Membrane Filtration Transfer Sample Immersion In Media Extraction of Bioburden Aerobic Bacteria Anaerobic Bacteria Fungal Bioburden Enumeration (sterile container) (shaker)
Sterility Test(ISO 11737-2:2009) Sample Immersion In Sterile Media Incubation (14 Days) Packaged Product (non-sterile) Pass Fail
Cycle Development • Processes developed are specific to product/packaging combination. • BIs placed in most difficult to kill location. • Product, load configuration and packaging fixed. Bioburden is monitored and controlled. • No surviving microorganisms after exposure to a reduced level of treatment (as per AAMI/ISO 14937). • Demonstration that BI is highly resistant to the sterilizing agent relative to the product bioburden (as per AAMI/ISO 14937).
Process Challenge Device http://bit.ly/Process-Challenge-Devices
Incubator Validation What’s different?
Chemical Indicators Warnings: These are not to be used instead of BIs Be careful how you store these
H202 Cycle Safety Margins – 4 Injection Dose Response Safety Half-Cycle Safety
Sterilization Validation Steps Material Compatibility Cycle Development (i.e., fractional cycles) Calibration & IQ 1 Fractional or Sub-lethal Cycle & 3 Half-Cycles 3 Full-Cycles
Incubation Reduction Study http://bit.ly/Incubation-Reduction Biological Indicator (BI) With Spores Incubation ≤80 BIs No Growth (3 lots min. of 100) • ≥30 BIs Fractional Cycle BI In Sterile Media Growth
UV Light http://bit.ly/Honle-UV Booth 760 – Honle UV America Inc. http://bit.ly/Lesco-UV Booth 1655 – American Ulraviolet
EtO in a Bag http://bit.ly/Anprolene Booth 3092 – Anderson Products
Noxilizer Booth #675 MDM West Michael Valentine VP, NA Sales
H2O2 Sterilizers VHP – Vapor Hydrogen Peroxide Gas Plasma http://bit.ly/Steris-Amsco Booth 2109 – Steris Isomedix