“ Parvobacteria ”
290 likes | 309 Vues
Explore the characteristics, culture requirements, pathogenicity, laboratory diagnosis, epidemiology, immunization, and treatment of Parvobacteria including Haemophilus, Bordetella, Brucella, and more. Learn about diseases like Meningitis, Bronchitis, Conjunctivitis, and more.

“ Parvobacteria ”
E N D
Presentation Transcript
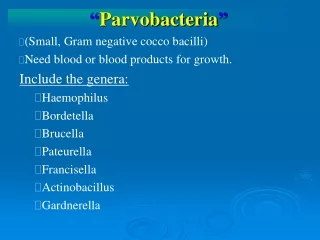
“Parvobacteria” (Small, Gram negative cocco bacilli) Need blood or blood products for growth. Include the genera: Haemophilus Bordetella Brucella Pateurella Francisella Actinobacillus Gardnerella
Haemophilus species • Gram negative coccobacilli • With pleomorphism- different shapes in Clinical specimens e. g. C.S.F Habitat: • Usually found in upper respiratory tract of man. • Culture • All species need blood or blood products for growth • Haemophilusinfluenzae can grow on: e.g. (A) Chocolate agar it contains both x and v factors
Haemophilus Influenzae (Cont.) (B) Blood agar with growth of Staphylococcus aureus – a phenomenon called satellitism Large colonies of H. influenzae near Staphylococcus colonies Small colonies of H. influenzae away from colonies of Staph. aureus Colonies of Staphylo- coccus aureus producing V factor Providing X Factor Blood Agar Plate
This is responsible for the phenomenon of “Satellitism” in which Hemophilus influenzae forms colonies in the vicinity of Staphylococcal colonies. BAP culture showing Haemophilus influenzae satelliting around Staphylococcus aureus, Picture from CDC.
c) On nutrient agar with: X Factor = Haematin and / or • V Factor = DI or TRI Nucleotide According to need for X, V OR XV Factors Haemophilus species can be divided into: Factor Required Species X and V H. influenzae, H. aegyptius H. haemolyticus X H. ducreyi V H. parainfluenzae, parahaemolyticus
Pathogenecity of Haemophilus species (Diseases) Species Disease H. influenzae capsulated Meningitis, arthritis, osteomyelitis, (mainly type a, b) cellulitis, epiglottitis, bacteremia H. influenzae non- Exacerbations of chronic bronchitis, capsulated sinusitis, otitis media, others. H. aegyptius Conjunctivitis H. ducreyi Chancroid (Sexually Transmitted) H. parainfluenzae Commensals of the upper H. Haemolytic Respiratory tract; rarely H. Parahaemolyticus Cause disease in immunocompromised patients
Haemophilus influenzae The most important pathogenic species: • Gram – negative coccobacilli • Growth on chocolate agar • Shows smooth drop like colonies on chocolate agar • Needs X and V factors for growth on nutrient agar • Shows satellalism near Staphyloccocusaureus colonies • Shows pleomorphism from clinical specimens egcsf • Divided into Capsulated and Non-capsulatedstrains.
Capsulated Strains • Capsule is made of Polysaccharides • It is antigenic • It increases the pathogenecity of strains • Prevents phagocytosis • Capsulated strains are divided into 6 Serotypes a b c d e f • Most pathogenic is type b.
H.influenzae invasive Infections (mainly by type B) Include: a) Meningitis b) Epilottitis c) Cellulitis d) Arthritis e) Osteomyelitis • Usually accompanied with bacteriaemia • Usually caused by type b • The major virulence factor is the polysaccharide capsule • Affects children between 3 months to 3 years. • Infection under two(2) months is rare because of presence of maternal IgG antibodies.
Laboratory Diagnosis Specimens depends on the type of diseases a. CSF – in meningitis b. Blood –meningitis and bacteriaemia and all types of invasive disease. c. Sputum – in pneumonia d. Swab – in cellulitis e. Synovial fluid – in arthritis • Direct smear shows pus cell + pleomorphic gram –ve coccobacilli • CSF Culture, on chocolate agar • CSF detection for presence of antigens by agglutination
Epidemiology of Invasive H. influenzae Infection • More common in winter after viral infection. • More common in crowded families with poor status. • Family members can infect each other. • Mortality is 5% • In meningitis neurological lesions - 10-15 % • Production of conjugate vaccine (Hib) reduced the morbidity and mortality.
Immunization • Early preparations consists of purified type b polysaccharide vaccines. But found not to be effective in children ↓18 months old. • Now conjugated vaccine which consist of polysaccharide combined with a carrier molecule, (which could be tetanus toxoid, non toxic diphtheria toxin or N. meningitidis components). This vaccine is protctive for children younger than 2 years.
Treatment • Ampicillin (amoxycillin) if not β lactamase Producer if β lactamase producer it destroy ampicillin and amoxycillin so use. • Chloramphenicol • Ceftriaxone,Cefuroxime • Chemoprophylaxis: Contacts of patient with H. influenzae type b infection can be given Rifampicin for 4 days as prophylaxis.
Hib Vaccine H = Haemophilus I = Influenzae B = Pittman type b Composition Polysaccharide + Carrier protein to increase antigenecity Carrier Protein • Toxoid of diphtheria • Toxoid non-toxogenic diphtheria • Toxoid of Tetanus • Outer Membrane protein of N. Meningitidis.
Hib (Contact) Total doses = 3 - 4 doses Starting at = 2/12 age Route = Intramuscular Effective after = 2/52 Not effective in = 1. HIV, antibodies deficiency 2. Asplenia, anatomical 3. Functional asplenia 4. Sickle cell disease 5. Bone marrow transplant 6. Therapy for malignancy
Non capsulatedstrains morphology is similar to capsulated strains. They cause: • Otitis media: presenting with pain and discharge of pus from the ear. b) Sinusitis: presenting with headache and postnasal discharge with low grade fever. c) Exacerbation of chronic bronchitis in elderly, smoking people presenting with cough and large amount of sputum.
( Cont. Non capsulated strains) • Pneumonia: mainly affecting both lungs called Bronchopneumonia. b) Bronchiectasis: collection of pus in dilated bronchi presenting with cough, chest pain, fever, and production of large amount of sputum
Bordetella pertussis And Bordetella parapertussis B. pertussis – causes WHOOPING COUGH B. parapertussis – causes a MILDER FORM OF WHOOPING COUGH. • Live mainly in the human respiratory tract. • Morphology: short, gram – negative coccobacilli.
MEDIA a. Bordet Gengue medium b. Charcoal blood agar BORDET – GENGUE CONTAINS: a. 30 % blood b. Penicillin c. Glycerol d. Penicillin WHY? To supress normal flora COLONIES look like mercury drops
ANTIGENIC STRUCTURE: Sharing 3 antigens 1, 2, 3 organism can carry TYPE 1, 2 antigens TYPE 1, 2, 3 antigens TYPE 1, 3 antigens
PATHOGENECITY – Strict human pathogen • Causes WHOOPING COUGH • Due to PRODUCTION OF ENDOTOXIN • which affect the respiratory mucosa.
Pathogenesis • Non invasive disease • Does not cause bacteremia • Human are the only natural host • Incubation period 1-2 weeks • Initial stage colonization of ciliated epithelium of the bronchi and trachea. • Production of cytotoxin which paralysis the cilia - so cough as the only protective mechanism • Production of pertussis toxin (PT) Lymphocytosis • Can also predispose to secondary bronchopneumonia.
Clinical Features a) Affect preschool children b) Severe in under 1 year of age c) An acute Tracheobronchitis Divided into 3 stages a) Catarrhal stage 2 / 52 - Fever - Rhinorrhoea, sneezing - Anorexia - Malaise
(Cont. 3 STAGES) b) Paroxysmal cough 2 / 52 -Violent cough followed by inspiratory (whoop) - Vomiting - Convulsions c) Convalences stage 4 / 52 -Leucocytosis (Lymphocytosis) can mimic lymphocytic leukemia.
Diagnosis a) Clinical b) Pernasal swab c) Cough plate d) Swab by Immunofluorescence (Rapid Method)
Treatment a) Erythromycin b) Effective on early stage c) Not effective in later stage WHY??
Vaccination 1. Whole killed bacterium vaccine 2. Give Intramuscularly as part of the Triple Vaccine DPT D = DIPTHERIA P = PERTUSSIS T = TETANUS 3. Safe but there are some cases of CNS involvement.
4. A cellular vaccine formed of a) PT = Pertussis toxin b) FHA = Filamentous haemagglutinin is supposed to be more save.
Complications Of Whooping (Cough) A) Bronchopneumonia - due to pyogenic cocci B) Bronchiatiasis C) Sub conjunctival haemorrgae