Valve selection
710 likes | 1.31k Vues
Valve selection. Weerachai Nawarawong M.D. Mechanical valve advantage. Children Patients <40 yrs High reoperation risk Small annular size Atrial fibrillation Pregnancy desired Patients > 70 yrs High thromboembolism risk High hemorrhage risk. Tissue valve advantage.

Valve selection
E N D
Presentation Transcript
Valve selection Weerachai Nawarawong M.D.
Mechanical valve advantage • Children • Patients <40 yrs • High reoperation risk • Small annular size • Atrial fibrillation • Pregnancy desired • Patients > 70 yrs • High thromboembolism risk • High hemorrhage risk Tissue valve advantage Akins CW: Ann Thorac Surg 1991,52:161-172
If one can choose the valve prosthesis one would choose: • “One valve for life”
Myths about Mechanical Valves • You’ll Never Need Another Operation • You can Live without Restrictions • Risks of TE/ACH are Minimal • Coumadin is Not a Problem
“Nine Commandmentsfor prosthetic valve” • Embolism Prevention • Durability • Ease and Security of Attachment • Preservation of Surrounding Tissue Function • Reduction of Turbulance • Reduction of Blood Trauma • Reduction of Noise • Use of Materials Compatible with Blood • Development of Methods of Storage and Sterilization
Ideal valve • Good hemodynamic • Quiet • Require no anticoagulation • Last for life time • Cheap • Easy to implant
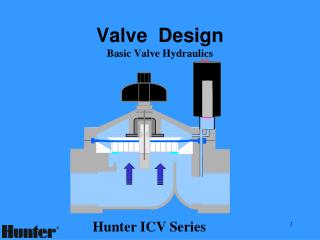
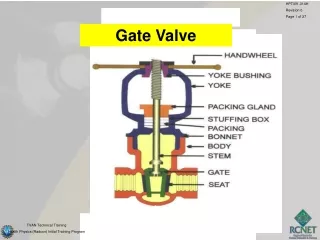
Valve Prosthesis • Mechanical • types: caged-ball, tilting-disk, bi-leaflet • advantage: durability • limitation: thrombogenicity • Bioprosthetic • types: heterografts, homografts • advantage: short term anticoagulation • limitation: structural failure • leaflet calcification & tissue degeneration leading to valvular regurgitation • rate of porcine valve degeneration 26% (aortic), 39% (mitral) in 10 yrs
Homografts • 1956 - first aortic valve homograft was used in the descending thoracic aorta for aortic regurgitation • 1962 - first sub-coronary use • high incidence of post-op failure * (years) 5 10 15 20 survival rate (%) 85 66 53 38 re-operation (%) 22 62 85 95 * Circulation 1991; 84(suppl 3):III81-III88
Durability and hemodynamic Bleeding and thromboembolism
Wall Street Journal 8//16//07 • Warfarin “is the second-most-likely drug, after insulin, to send Americans to the emergency room”. • By one estimate, it accounts for 43,000 ER visits a year in the U.S.
Van der Meer: • 42% more major bleeding complications for every one-point increase in INR. • The incidence from major bleeding complications given in the literature varies between 1.6% and 5.2 % increasing with age
Incidence of major embolismafter mechanical valve replacement • Absence of antithrombotic therapy • 4% per year • plus 1.8% per year risk of valve thrombosis • Antiplatelet therapy • 2.2% per year • plus 1.6% per year risk of valve thrombosis • Wafarin therapy • 1% per year • 0.8% per year with an aortic valve • 1.3% per year with a mitral valve • plus 0.2% per year risk of valve thrombosis • Incidence of major bleeding in patients treated with warfarin • 1.4 per 100 patient-years. (Circulation. 1994;89:635-641.)
Incidence Rates of Valve Thrombosis and Major and Total Embolisms: Effect of Antithrombotic Treatment Incidence Rates per 100 Patient-Years (95% Confidence Intervals) Anticoagulation Valve Thrombosis Major Embolism Total Embollsm* None 1.8 (0.9-3.0) 4.0 (2.9-5.2) 8.6 (7.0-10.4) Antiplatelet 1.6 (1.0-2.5) 2.2 (1.4-3.1) 8.2 (6.6-10.0) Dipyridamole 4.1 (1.9-7.2) 5.4 (2.8-8.8) 11.2 (7.3-15.9) Aspirin 1.0 (0.4-1.7) 1.4 (0.8-2.3) 7.5 (5.9-9.4) Coumadin 0.2 (0.2-0.2) 1.0 (1.0-1.1) 1.8 (1.7-1.9) Coumadin and antiplatelet 0.1 (0.0-0.3) 1.7 (1.1-2.3) 3.2 (2.4-4.1) (Circulation. 1994;89:635-641.)
Incidence Rates of Valve Thrombosis and Major and Total Embolisms With Coumadin Therapy: Effect of Valve Position Incidence Rates per 100 Patient-Years (95% Confidence Intervals) Valve Position Valve Thrombosis Major Embolism Total Embolism* Aortic 0.1 (0.1-0.2) 0.8 (0.7-0.9) 1.1 (1.0-1.3) Mitral 0.5 (0.3-0.7) 1.3 (1.1-1.5) 2.7 (2.3-3.0) Both 0.4 (0.2-0.7) 1.4 (1.0-1.9) 2.1 (1.6-2.7) (Circulation. 1994;89:635-641.)
Types of prosthetic valves and thrombogenicity Type of valve Model Thrombogenicity Mechanical Caged ball StarrEdwards + + + + Single tilting disc BjorkShiley, Medtronic Hall + + + Bileaflet St Jude Medical, Sorin Bicarbon, Carbomedics + + Bioprosthetic Heterografts CarpentierEdwards, Tissue Med (Aspire), Hancock II + to + + Homografts +
Mitral heart valve prostheses carry a risk of embolism that is almost twice as high as aortic valve prostheses • Cannegieter SC, Rosendaal FR, Briet E (1994) Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses. Circulation 89 :635–641
Zellner et al “Long term experience With the St.Jude Medical Valve Prosthesis” South Carolina,USA AVR 418 pts, mean age 54.8yrs Re-operation inc. 1.0%/pt/y
Gradient Comparison of mean pressure gradients for commonly implanted prosthetic valves.
EOA Comparison of EOAs for commonly implanted prosthetic valves.
There are trends in the United States and Europe toward the increasing use of tissue rather than mechanical valves and toward the use of bioprostheses in progressively younger patients • Dagenais F, Cartier P, Voisine P, Desaulniers D, Perron J, Maillot R, Raymond G, Métras J, Doyle D, Mathieu P. Which biologic valve should we select for the 45- to 65-year-old age group requiring aortic valve replacement? J Thorac Cardiovasc Surg. 2005;129:1041–1049.
Reasons for increasing use of Bioprosthesis • Newer generation bioprosthesis are more durable and better. • Reoperation rates for patients over 65 years of age are particularly low with modern stented bioprostheses • The risks of reoperation have continued to decrease • Patients undergoing AVR today are older population than those studied in the randomized trials. • Young patients undergoing aortic valve surgery are often reluctant to accept warfarin therapy and the activity constraints associated with anticoagulants. • There are some nonrandomized but relatively large comparative trials that have shown apparent survival benefit for patients receiving bioprostheses, particularly for those over the age of 65 years .
Why bioprosthesis • Better fixation technique • Better anticalcification technique • Better long term result in newer generation valve • Better surgical technique , redo less dangerous
Two historic randomized clinical trials compared outcomes after valve replacement with a first-generation porcine heterograft and the original Bjork-Shiley tilting-disc mechanical valve: • The Edinburgh Heart Valve Trial, conducted between 1975 and 1979 with an average follow-up of 12 years, • The Veteran Affairs (VA) Cooperative Study on Valvular Heart Disease, conducted between 1979 and 1982 with an average follow-up of 15 years.
The Edinburgh trial • a small survival advantage associated with a mechanical valve in the aortic but not in the mitral position; • both trials showed • increased bleeding associated with mechanical valves • increased reoperation with tissue valves; • structural failure of tissue valves and overall thromboembolic complications were greater after mitral than after aortic valve replacement.
A meta-analysis of 32 articles evaluated mortality from 15 mechanical and 23 biological valve series including 17,439 patients and 101, 819 patient-years of follow-up. • no difference in riskcorrected mortality between mechanical and bioprosthetic aortic valves regardless of patient age • choice between a tissue and mechanical valve should not be based on age alone. • Lund O, Bland M. Risk-corrected impact of mechanical versus bioprosthetic valves on long-term mortality after aortic valve replacement. J Thorac Cardiovasc Surg. 2006;132:20 –26.
Retrospective study comparing mechanical and tissue aortic valve replacement in 3062 patients with combined follow-up of 22 182 patientyears • age but not valve type was predictive of valve-related mortality. • reoperation was higher after tissue aortic valve replacement only for patients ≤60 years of age, • combined valverelated morbidity was higher after mechanical valve replacement for all patients 40 years of age. • Chan V, Jamieson WRE, Germann E, Chan F, Miyagishima RT, Burr LH, Janusz MT, Ling H, Fradet GJ. Performance of bioprostheses and mechanical prostheses assessed by composite of valve-related complications to 15 years after aortic valve replacement. J Thorac Cardiovasc Surg. 2006;131:1267–1273.
Advances in tissue fixation and anticalcification treatment have resulted in current-generation bioprostheses that have superior durability
Freedom from structural valve deterioration • Carpentier-Edwards pericardial aortic valve (age 65) • 94% at 10 years • 77% at 15 years • 10% chance that a 65-year-old patient would require reoperation before 80 years of age. • Third-generation bioprostheses may be even more durable, with • 92.8% at 12 years (mean age of 54 years) • In addition, advances in myocardial protection and cardiac surgical techniques have led to lower risks at reoperation, making the prospect of redo valve surgery less dangerous. • Banbury MK, Cosgrove DM III, White JA, Blackstone EH, Frater RWM, Okies JE. Age and valve size effect on the long-term durability of the Carpentier-Edwards aortic pericardial bioprosthesis. Ann Thorac Surg. 2001;72:753–757. • Bach DS, Metras J, Doty JR, Yun KL, Dumesnil JG, Kon ND. Freedom from structural valve deterioration among patients 60 years of age and younger undergoing Freestyle aortic valve replacement. J Heart Valve Dis. In press.