INTERDISCIPLINARY MODELS OF INTEGRATED CARE
180 likes | 541 Vues
INTERDISCIPLINARY MODELS OF INTEGRATED CARE. PATIENT CENTERED CARE ALIGNING AND BUILDING COMPETENCE WITH PRIMARY CARE PROVIDERS RAY SOUSA, MAPC, LPC . WELCOME!. INTRODUCTIONS WHAT DOES THE CLINICAL “LANDSCAPE” LOOK LIKE IN YOUR CLINICAL SETTING? AN IMAGE?.

INTERDISCIPLINARY MODELS OF INTEGRATED CARE
E N D
Presentation Transcript
INTERDISCIPLINARY MODELS OF INTEGRATED CARE PATIENT CENTERED CARE ALIGNING AND BUILDING COMPETENCE WITH PRIMARY CARE PROVIDERS RAY SOUSA, MAPC, LPC
WELCOME! • INTRODUCTIONS • WHAT DOES THE CLINICAL “LANDSCAPE” LOOK LIKE IN YOUR CLINICAL SETTING? • AN IMAGE?
“MENTAL HEALTH AND PHYSICAL HEALTH ARE CLOSELY CONNECTED. MENTAL HEALTH PLAYS A MAJOR ROLE IN PEOPLE’S ABILITY TO MAINTAIN GOOD PHYSICAL HEALTH. MENTAL ILLNESS, SUCH AS DEPRESSION AND ANXIETY, AFFECT PEOPLE’S ABILITY TO PARTICIPATGE IN HEALTH-PROMOTING BEHAVIORS. IN TURN PROBLEMS WITH PHYSICAL HEALTH, SUCH AS CHRONIC DISEASES, CAN HAVE A SERIOUS IMPACT ON MENTAL HEALTH AND DECREASE ABILITY TO PARTICIPATE IN TREATMENT AND RECOVERY” HEALTHYPEOPLE.GOV
WILL IT BE A “SHOTGUN WEDDING A BLESSING OR BOTH!? • PATIENT CENTERED CARE IS THE GUIDING PRINCIPLE OF COLLABORATION • WHERE IS YOUR INSTITUTION ON THE INTERDISCIPLIARY CONTINUIM? • THE AFFORDABLE CARE ACT MANDATESSOME FORM OF MENTAL HEALTH CARE.
CERTIFIED PATIENT-CENTERED MEDICAL HOME NCQA • ENHANCED ACCESS AFTER HOURS AND ONLINE • LONG-TERM PATIENT AND PROVIDER RELATIONSHIPS • SHARED DECISION MAKINGERTIFIED • CASE MANAGER • SUPPORT STAFF • TEAM BASED CARE • BETTER QUALITY AND EXPERIENCE • LOWER COST FROM RFEDUCED EMERGANCY DEPARTMENT AND HOSPITAL USE
A PHYSICIAN SPEAKS CANDIDLY • “We are talking about a …malignant view of physicianhood which ignores, indeed attacks, the rights and needs of physicians themselves to be sensitive, to feel pain, to be human beings. Doctors are taught and then reinforced in countless ways that they should hold feelings in, go it alone, never let their vulnerability show”… Medicine as a Human Experience, Reiser & Rosen, 1984
TALKING TO PRIMARYPROVIDERS: RULES OF THE ROAD • TREAT THEM EQUALLY – WITH YOURSELF AND EACH OTHER • Read Medscape and other blogs • Familiarize yourself with their changing world • Don’t play the expert but you should know how your care impact the health issues of their patients i.e.. Asthma, diabetes, hypertension, chronic pain. • Get to know the benchmarks for treating these diseases • Acknowledge referrals with a summary of your clinical impressions and plan. • People with mental illness die much earlier than those without. Providers need your help knowing how to identify them. • Get them engaged in care and help keep them well • Figure out where providers fit in the reimbursement hierarchy. That will explain many of their frustrations. • If your agency doesn’t have an EMR talk to your peers about what they are using. Take a workshop. • Paper notes are on their way out. Undocumented treatment is already out.
Clinical Experience • PATIENTS OFTEN GO TO THEIR PRIMARY CARE PHYSICIAN FOR ISSUES WHICH ARE REALLY BEHAVIOR HEALTH ISSUES • IT IS CRITICAL THAT THE CARE TEAM SEES BEHAVIOR HEALTH AS ESSENTIAL TO THE INTERDISCIPLINARY CARE TEAM • ISSUES OF ADDICTION ARE OFTEN BEST FIRST ADDRESSED BY BEHAVIOR HEALTH • THE ELECTRONIC RECORD IS AN IDEAL WAY FOR YOU AND THE PHYSICIAN TO COMMUNICATE AND ADJUST THE ONGOING CARE PLAN
OUR ENCOUNTERS WITH OUR CLIENTS DO AT LEAST TWO VITAL THINGS: PROVISION OF CARE AND ALWAYS PROMOTING AND PROVIDING NEEDED EDUCATION FOR WELLNESS. • WHEN DONE EFFECTIVELY, WE MAKE THE WORK OF THE PHYSICIAN EASIER! DOCS LOVE THAT! • ONSITE BEHAVIOR HEALTH REDUCES LACK OF FOLLOW THROUGH BY PATIENTS. • A SUPPORTIVE COMMUNITY FOR BEHAVIOR HEALTH IS VERY IMPORTANT.
BEING A CLINICIAN AND SPIRITUAL CARE • WE ARE MOVING TO NEEDING TO BE BOTH A LICENSED CLINICAN AND HAVE CHAPLAIN EXPERTISE • POLLS SHOW THAT PATIENTS WANT TO INCOARPORATE SPIRITUALITY IN THEIR CARE IN A WAY THAT INCLUDES THE PHYSICIAN • THE OPPOSITE OF PLACEBO – “NOCEBO” • GOOD MEDICINE IS ALL ABOUT RELATIONSHIP • Unfortunately, if that relationship is one of insensitivity, or neglect, the relationship becomes the Nocebo* as described by Nicholas Wade: “Much less attention has been paid to the inverse of the placebo effect, the creation of expectancies that make people worse.” (The Spin Doctors by Nicholas Wade Pg.16 (The New York Times Magazine)
ACCESS COMMUNITY HEALTH NETWORK INFECTIOUS DISEASE CLINIC STRUCTURE • THERE ARE 34 “HUB SITES” WITHIN THE NETWORK • ALL ARE LOCATED IN NEIGHBORHOODS WHERE THERE IS HEALTH CARE DISPARITY • EXTENSIVE OUTREACH TO AT RISK POPULATIONS • CONSUMER ADVISORY BOARD • PATIENT ADVOCATES
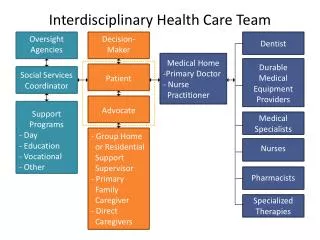
CARING FOR OUR HIV+ CLIENTS The Team • THE INFECTIOUS DISEASE PHYSICIAN • SUPPORTING MEDICAL STAFF: • NURSES, PHYSICIAN ASSISTANT, MEDICAL, BEHAVIOR HEALTH CONSULTANTS, PSYCHIATRY, CHAPLAINS, ASSISTANTS, CASE MANGERS, PATIENT ADVOCATES, ADDICTION SPECIALISTS.
HIV ISSUESS FOR BEHAVIOR HEALTH • BEHAVIOR HEALTH IS AN ESSENTAL PART OF THE CARE OF OUR HIV PATIENTS. • REGULAR ASSESSMENT BY OUR “BHC” • REFERRRAL BY THE TREATING DOCTOR. • CONSULTATION WITH THE DOCTOR CONCERNING ABOUT HOW THE PATIENT IS COPING AND WHAT THE CARE PLAN WILL BE.
FREQUENTLY OCCURING CLINICAL ISSUES • THE MANNER IN WHICH THE INFECTION WAS CONTRACTED • HOW LONG HAS THE PATIENT BEEN UNTREATED? • WHAT IS THE EXTENT OF THEIR DISCLOSURE OF THEIR HIV STATUS? • IS THERE A SUPPORT NETWORK IN PLACE? • HOW MUCH DOES THE PATIENT KNOW ABOUT HIV?
ADDRESSING STIGMA AND DISCRIMINATION • STIGMA IS AN ATTITUDE • DISCRIMINATION IS A BEHAVIOR WHICH FLOWS FROM STIGMA. • “I AM MORE RELIGIOUS THAN GAY!” • THE DEMOGRAPHIC SHIFT LINKING HIV MORE TO POVERTY, RACE AND MINORITIES. • CALLS FOR ONGOING CULTURAL SENSITIVITY • THE ROLE OF FAITH COMMUNITIES
FAITH BASED COMMUNITY CLINICS • PHYSICIAN INVOLVEMENT FROM THE VERY BEGINNING • THEY BRING WITH THEM MEDICAL STAFF, EQUIPMENT ETC. THAT YOU CANT PROVIDE. • THE CONGREGATION KNOWS THE COMMUNITY AND ITS NEEDS. • ESTABLISHING AND MAINTAINING GOOD RELATIONSHIPS WITH LOCAL ALDERMEN AND OTHER PERTINENT LOCAL OFFICIALS. • STRONG LEADERSHIP IS NEEDED IN ORDER TO MAINTAIN RELATIONSHIPS BETWEEN MEDICAL STAFF AND CONGREGATIONAL COMMITTEES WHO HAVE THEIR OWN RYTHMN WHICH MAY SEM SLOWER.
KNOW YOUR TARGET POPULATION • What is their insurance status? • Do Good Samaritan laws apply for the protection of the medical and behavior health staff? • Is their a billing process? Sliding scale? • Identified local resources: local food pantries and other pertinent social services. • Avoid the “Lone Ranger” syndrome! • It first and last a community enterprise! • Identify your spiritual understand of suffering and healing and social justice. • ocia
“MENTAL HEALTH AND PHYSICAL HEALTH ARE CLOSELY CONNECTED. MENTAL HEALTH PLAYS A MAJOR ROLE IN PEOPLE’S ABILITY TO MAINTAIN GOOD PHYSICAL HEALTH. MENTAL ILLNESS, SUCH AS DEPRESSION AND ANXIETY, AFFECT PEOPLE’S ABILITY TO PARTICIPATGE IN HEALTH-PROMOTING BEHAVIORS. IN TURN PROBLEMS WITH PHYSICAL HEALTH, SUCH AS CHRONIC DISEASES, CAN HAVE A SERIOUS IMPACT ON MENTAL HEALTH AND DECREASE ABILITY TO PARTICIPATE IN TREATMENT AND RECOVERY” HEALTHYPEOPLE.GOV