"My urine flow is poor”
220 likes | 435 Vues
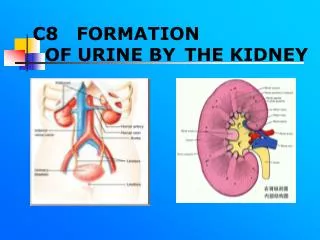
"My urine flow is poor”. Shane is 65-years old and complains of a 4 to 5-month history of progressive difficulty voiding. He finds it difficult to start urinating and when he does go he has the feels as though he hasn't emptied his bladder completely.

"My urine flow is poor”
E N D
Presentation Transcript
Shane is 65-years old and complains of a 4 to 5-month history of progressive difficulty voiding. • He finds it difficult to start urinating and when he does go he has the feels as though he hasn't emptied his bladder completely. • Consequently, after voiding he often feels as though he needs to urinate again. He denies any burning, urgency or urethral discharge.
DxT: poor urine flow + straining to void + frequency = BOO • Bladder outlet obstruction • Prostate cancer • BPH • Prostatitis • Prostatic stones
Q2 What issues in the history of a patient presenting with LUTS would you seek to support a particular diagnosis?
Is there a history of some weeks or months of bladder irritability (urinary frequency, nocturia)? Exclude urinary tract infection if the history is short or if dysuria is a major feature. Remember that acute urinary tract infection may be the first sign of prostate cancer • Is there a history of difficulty stopping or starting urination, and is the strength of the urine stream deteriorating? These are cardinal symptoms of prostatic enlargement and may not necessarily indicate prostate cancer • Is there any bone pain? Prostate cancer often spreads to the bones early, and bone pain may be the first symptom. The pain is usually localized, constant, and severe, and it may be worse with movement • Is there any pain on ejaculation or blood in the ejaculate? These symptoms do not necessarily indicate any disease, but they may indicate prostatitis as well as prostate cancer • Is the patient feeling generally unwell or tired, or has there been any weight loss, anorexia, thirst, memory disturbance, or confusion—perhaps noted by family or friends? These nonspecific features indicate possible systemic disease from cancer dissemination, renal failure, or hypercalcemia
Is there any lower limb numbness or weakness, difficulty walking, or problems with emptying the bowels or bladder? These features all suggest possible spinal cord problems and warrant rapid, complete investigation Family history • Has anyone in your family ever had any prostate trouble? First-degree relatives are of particular interest • Has anyone in your family undergone prostate surgery? Determine if this was for cancer or for BPH • Does anyone in your family have regular injections for his prostate? Likely to be goserelin
Q3 What risk factors are thought to be important in the development of carcinoma of the prostate?
Advanced age • Family history • The presence of BRCA1 or BRCA2 mutations increases the risk of developing prostate cancer • African-American ethnicity • High dietary saturated fat intake, especially α-linolenic acid (found in red meat and butter), may be a risk factor and is crudely estimated to account for 10% to 15% of geographic differences in incidence. In contrast, genistein, an isoflavone found in soy, is believed to be protective (it inhibits 5α-reductase) • Low vegetable diet • Vasectomy has been proposed as a risk factor, but a large analysis found no relationship, and the American Urological Association states that vasectomy is not associated with increased risk
Digital rectal examination (DRE) may reveal a nodule (50% are not carcinoma). Locally advanced cancer typically reveals a hard, nodular and irregular gland. • Plus the usual….
All about PSA (not Pharmaceutical Society of Australia)
What is PSA? • Prostate Specific Antigen (PSA) is a glycoprotein actually not there to help screen for prostate pathology but to act physiologically in the ejaculate to liquefy the semen allowing sperm to break free from their seminal coagulum prison and swim freely; is likely to be instrumental in dissolving the cervical mucous via its proteolytic qualities, allowing the entry of sperm. • PSA leaks into serum normally, and is present in the circulation of healthy men. Various prostate pathology will increase PSA eg. Prostatitis, BPH, Prostate CA etc. So PSA serum levels are used as a screening test.
What are some of the factors that can affect PSA levels? • PSA has not diurnal variation. Normal healthy males’ PSA levels don’t change. • Ejaculation increases PSA levels, but they return to normal within 24 hours • Some say riding pushbikes and motorbikes increases PSA too, but evidence remains inconclusive. • Some drugs like cyclophosphamide and others can increase PSA too. • DRE gives no significant change in PSA. BUT a vigorous prostate massage can produce a short-term 2-fold increase….Nothing sus. • Cystoscopy, urethral catheterization, and TRUS do not tend to elevate the PSA level. • Prostate needle biopsy increases PSA by a median of 7.9 ng/mL (6.5 times baseline value) within 5 minutes following the biopsy, this persists for 24 hours. • Urinary retention increases PSA levels, but when relieved, they decrease 50% in 24-48 hours. • Acute prostatitis produces large increases in PSA, but the return to baseline depends on resolution of the infection, which may take 6-8 weeks or longer. PSA levels have been used to determine the duration of antimicrobial therapy in men with acute bacterial prostatitis. • PSA half-life is 2.2-3.2 days. After a biopsy, 2 to 4 weeks may need to elapse before the PSA returns to its original level.
What investigations would be most helpful and why? • DRE of course - Although PSA testing detects more cancers than DRE, a combination of the 2 methods is better: DRE detects more cancers at the PSA cutoff of 4.0 ng/mL, but this may not occur if the cutoff is lowered to 3.0 ng/mL. In men with prostate cancer whose PSA level was less than 4 ng/mL, normal DRE findings were present in 4-9%, while DRE findings were positive in 10-20%. When the PSA level was greater than 4 ng/mL, negative DRE results were found in 12-32% of patients, while positive DRE results were present in 42-72% of patients. • TRUS Biopsy • Cancer markers in general… Alkaline phosphatase • Other Prostate cancer markers… Human glandular kallikrein–2 Prostate-specific membrane antigen Cell cycle inhibitor p27 Serum insulinlike growth factor
Few issues in medicine are as controversial as screening for prostate cancer. Briefly discuss why this is the case.
Few issues in medicine are as controversial as screening for prostate cancer. Briefly discuss why this is the case. • PSA testing it has a Positive predictive value of about 35% when the cutoff is about 3ng/mL (but we normally have cutoff at 4ng/mL • PSA testing with a cutoff of 4 ng/mL has a sensitivity of 67.5-80% implies that 20-30% of cancers are missed when only the PSA level is obtained. The sensitivity can be improved by lowering the cutoff or by monitoring PSA values so that a rise in PSA level of more than 20-25% per year or an increase of 0.75 ng/mL in a year would trigger performance of a biopsy regardless of the PSA value. • The specificity of PSA at levels greater than 4 ng/mL is 60-70%. Specificity can be improved by using age-adjusted values, • Men with low readings might still harbor dangerous cancers (gleason stage 5 might not produce PSA anymore), while those with high readings might be completely healthy. • PSA, while normally at a steady serum concentration, can be affected by a lot of things (see above) • Studies have shown that screening does not reduce the death rate in men 55 and over. • NNT = 48 That’s 47 men who, in all likelihood, can no longer function sexually or stay out of the bathroom for long because the PSA test was justification for a urologist to jab it. • More suited to monitor remission of prostate cancer etc
If screening is to be carried out which patients might be targeted and why?
If screening is to be carried out which patients might be targeted and why? • Don’t screen for prostate cancer in men aged 75 years or older – they will die WITH CA rather than FROM it Screening when male and: • 40yrs + family Hx of prostate CA or proven BRCA1/2 etc • 50yrs + No family Hx • recent onset of LUTS