Neuropathic Pain
400 likes | 802 Vues
Neuropathic Pain. Pain Pathophysiology. Nociceptive pain Neuropathic pain . Nociceptive Pain. Sensitization and activation of “healthy” nociceptor endings and recruitment of “silent” nociceptors

Neuropathic Pain
E N D
Presentation Transcript
Pain Pathophysiology • Nociceptive pain • Neuropathic pain
Nociceptive Pain • Sensitization and activation of “healthy” nociceptor endings and recruitment of “silent” nociceptors • “Soup” of inflammatory algogenic agents, such as protons, prostaglandins, bradykinin, serotonin, adenosine, histamine, cytokines
Mechanisms of Neuropathic Pain • Noninflammatory states • Inflammatory states
Pathophysiology of Neuropathic Pain • Ectopic activity in the peripheral pathways, including axons and DRG • CNS mechanisms
Neuropathic Pain: Central Mechanisms Peripheral neuropathic events can be complicated by temporary or long-term CNS changes, such as central sensitization and then reorganization of the pain pathways at the dorsal horn level
Neuropathic Pain and SMP • Some neuropathic pains are sustained, at least in part, by sympathetic efferent activity • SMP • Expression of alpha-adrenergic receptors on injured C-fibers may be a relevant mechanism of SMP, but others are possible • Clinical findings consistent with CRPS signal an increased likelihood of SMP
Nociceptive Pain Neuropathic Pain PNS peripheral nervous system PNS Peripheral sensitization “Healthy” nociceptors Abnormal nociceptors CNS central nervous system CNS Central sensitization Normal transmission Central reorganization Physiologic state Pathologic state Pappagallo M. 2001.
Neuropathic Pain • Diverse syndromes with uncertain classification • Mononeuropathies and polyneuropathies • CRPS • Deafferentation syndromes, including central pain
Painful Mononeuropathies and Polyneuropathies • Diabetic neuropathies • Entrapment neuropathies • Shingles and postherpetic neuralgia • Trigeminal and other CNS neuralgias • HIV-related neuropathy • Neuropathy due to malignant disease • Neuropathy due to rheumatoid arthritis, systemic lupus erythematosus, Sjögren’s syndrome • Idiopathic distal small-fiber neuropathy
Painful Mononeuropathies and Polyneuropathies • Neuropathies due to toxins: arsenic, thallium, alcohol, vincristine, cisplatinum, didioxynucleosides • Amyloid polyneuropathy: primary and familial • Neuropathies with monoclonal proteins • Vasculitic neuropathy • Neuropathy associated with Guillain-Barré syndrome • Neuropathy associated with Fabry’s disease
Neuropathic Pain: Clinical Assessment • A comprehensive diagnostic approach to patients affected by neuropathic pain • Medical history • Examinations: general, neurologic, regional • Diagnostic workup: imaging studies, laboratory tests, nerve/skin biopsies, electromyography/nerve-conduction velocity (EMG-NCV) studies, selected nerve blocks
Medical History Ask patient about complaints suggestive of • Neurologic deficits: persistent numbness in a body area or limb-weakness, for example, tripping episodes, inability to open jars • Neurologic sensory dysfunction: touch-evoked pain, intermittent abnormal sensations, spontaneous burning and shooting pains
Neurologic and Regional Examinations In patients with neuropathic pain, examination should focus on the anatomic pattern and localization of the abnormal sensory symptoms and neurologic deficits
Neuropathic Pain: Clinical Characteristics • Burning, shooting, electrical-quality pain • May be aching, throbbing, sharp • Neuropathic sensations: dysesthesias, paresthesias
Neuropathic Sensations • Paresthesias: abnormal; spontaneous, intermittent, painless • Dysesthesias: abnormal; spontaneous or touch-evoked, unpleasant
Neuropathic Pain: Evoked Dysesthesias • Allodynia: pain elicited by a nonnoxious stimulus (clothing, air movement, touch) • Mechanical (induced by light pressure) • Thermal (induced by a nonpainful cold or warm stimulus) • Hyperalgesia: exaggerated pain response to a mildly noxious (mechanical or thermal) stimulus • Hyperpathia: delayed and explosive pain response to a noxious stimulus
Primary Hyperalgesia • Present in the primary zone, at the location of injury • Characterized by pinprick hyperalgesia + warm and heat hyperalgesia + static mechanical allodynia (tenderness) • Indicative of PNS sensitization
Secondary Hyperalgesia • Present in the zone surrounding an injury • Characterized by dynamic mechanical allodynia + cold hyperalgesia • Indicative of CNS sensitization
Diagnostic Workup: Lab Tests • Complete blood cell count with differential, erythrocyte sedimentation rate, chemistry profile • Thyroid-function tests, vitamin B12 and folate, fasting blood sugar, and glycosylated hemoglobin • Serum protein electrophoresis with immunofixation • Lyme titers, hepatitis B and C, HIV screening • Antinuclear antibodies, rheumatoid factor, Sjögren’s titers (SS-A, SS-B), antineutrophil cytoplasmic antibody
Diagnostic Workup: Lab Tests • Cryoglobulins • Antisulfatide antibody titers, anti-HU titers • Heavy metals serum and urine screens • Cerebrospinal fluid study for demyelinating diseases and meningeal carcinomatosis
Diagnostic Workup: Electrophysiologic Studies EMG-NCV and QST • To localize pain-generator/nerve or root lesion • To rule out • Axonal vs focal segmental demyelination • Underlying small-fiber or mixed polyneuropathy
Biopsies • Nerve (eg, sural nerve): to diagnose vasculitis, amyloidosis, sarcoidosis, etc. • Skin: to evaluate density of unmyelinated fibers within dermis and epidermis
Neuropathic Pain: Management • Pharmacotherapy • Nonopioid • Opioid • Adjuvant analgesics • Interventional • Neural blockade (eg, sympathetic nerve blocks) • Neurostimulatory techniques (eg, spinal cord stimulation) • Intraspinal infusion
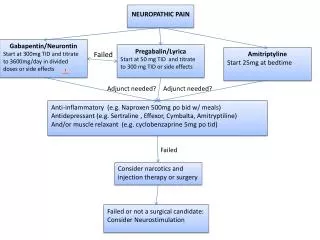
Neuropathic Pain:Pharmacologic Therapies • Gabapentin, carbamazepine, lamotrigine, and newer AEDs • Antidepressants • Opioid analgesics • Lidocaine (transdermal, intravenous [IV]), mexiletine • Alpha-2 adrenergic agonists
Neuropathic Pain: Management • Rehabilitative approaches • Psychologic interventions
Conclusions • More effective medical therapies for neuropathic pain are becoming available and physicians should use them to limit unnecessary suffering, with the ultimate goal of significantly improving patients’ quality of life