Understanding Renal Failure in Children: Causes, Symptoms, and Treatment
700 likes | 809 Vues
This comprehensive guide provides insights into renal failure in children, covering causes, symptoms, and essential treatment methods. Learn about normal kidney function, renal insufficiency, and basic manifestations to recognize and address renal issues in young patients. Explore acute renal failure, primary and secondary renal diseases, and the dysfunctions in excretion and endocrine functions of the kidneys. Enhance your knowledge of diagnosing and managing renal conditions in children with this informative resource.

Understanding Renal Failure in Children: Causes, Symptoms, and Treatment
E N D
Presentation Transcript
患儿女,11月。因呕吐、腹泻伴发热9天,无尿5天入院。患儿女,11月。因呕吐、腹泻伴发热9天,无尿5天入院。 • 9天前无诱因出现腹泻,每天3~4次,伴频繁呕吐,非喷射状,量较多;同时发热,体温最高41℃。给予口服抗生素治疗,三天后腹泻、呕吐次数减少,但体温仍在38~39℃之间。近5天一直无尿。体检:呼吸60次/分,脉搏120次/分,血压85/54mmHg。昏睡状态。双眼睑及球结膜水肿,睑结膜稍苍白,口唇干裂,咽充血,颈无抵抗;呼吸深大。 • 实验室检查:便常规正常;血钾8.6mmol/L,血钠128mmol/L,氯化物100mmol/L, 血钙1.98mmol/L,血磷2.33mmol/L, 尿素氮37.12mmol/L,血肌酐804.44μmol/L;血气分析:pH7.17, PCO224.5mmHg, HCO3-8.6mmol/L, • SBE -18.3mmol/L;心电图:室内传导阻滞,T波高尖。
§1 Introduction • Normal function of the kidney • Renal insufficiency • Causes • Basic manifestation of renal insufficiency
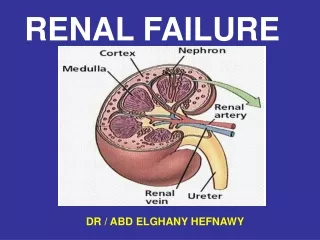
Normal function of the kidney 1.Excretion Remove waste product from the body; Regulate electrolyte and acid-base balance. 2. Endocrine Produce renin、EPO、1,25(OH)2D3 and prostaglandins; Inactivate gastrin、PTH.
Renal insufficiency Dysfunction of excretion and endocrine Diseases Symptoms and signs Edema, hypertension, oliguric, polyuria, hematuria, proteinuria, anemia, osteodystrophy.
Causes: 1 Primary renal diseases Primary glomerular diseases, Primarytubulardiseases, Interstitial nephritis, et al. 2 Secondary renal lesion Circulatory system diseases, immunity siseases, metabolic diseases, hematopathy, et al.
Basic manifestation of renal insufficiency • 1 Glomerular dysfunction • 2 Tubular dysfunction • 3 Endocrine dysfunction
1 Glomerular dysfunction • ①GFR • ⅰblood flow • ⅱnet filtration pressure • ⅲ Kf • ② Glomerular permselectivity
2 Tubular dysfunction ①proximal tubule Renal glycosuria, aminoaciduria, renal tubular acidosis, hypophosphatemia ②loop of Henle Hypotonic or isotonic urine, polyuria ③distaltubule Acid-base and electrolyte disorders, polyuria
3 Endocrine dysfunction ① Renin ②Endothelins ③KKS disorders ④AA Disequilibrium ⑤EPO ⑥ 1,25(OH)2D3
Excretion §2 Acute renal failure Conception Diseases water intoxication,azotemia, hyperkalemia, metabolic acidosis
Section 1 Cause and Classification *** Classification 1causes Prerenal ~ Intrarenal ~ Postrenal ~ 2renallesion functional~ organic~ obstructive ~ 3urine volume Oliguric ~ Nonoliguric ~
1 Prerenal factor renal blood flow Characteristic early stage: functional~ late stage: organic ~ (2) oliguria Causes
Mechanism ECF↓ RBF ↓ GFR↓ Reabsorption↑ oliguria Impaired homeostasis
Causes (1) acute tubular necrosis,ATN 2/3 acute renal ischemia acute renal poisoning hemoglobinuria, myoglobinuria (2) renal disease Characteristic (1) parenchymal (2) oliguric ~ nonoliguric~ 2intrarenal factor
Differentiation between the two RF urine functionalRForganic RF specific gravity> 1.020 < 1.015 OP(mmol/L) > 700 < 250 Na(mmol/L)< 20 > 40 UrCr/SrCr > 40 < 20 Sedimentnormal Manicol testurine volumeurine volume Necrosis epithelial cells,RBC,casts, albuminuria
Causes Kidney stone, tumor, obstruction of necrosis tissue Characteristic early stage: obstructive ~ late stage: organic ~ 3 Postrenal factor
Mechanism Bowman’s capsule pressure↑ Obstruction of the urinary tract Net filtration pressure↓ GRF↓ Oliguria, anuria
Section 2 Pathogenesis 1Glomerular factor ①RBF (1) Net filtration pressure BP < 60mmHg CO RBF BP (50-70mmHg) GFR (1/2 – 2/3) BP(40mmHg) GFR = 0 Urinary obstruction intracapsular pressure
afferent arteriole constriction efferent arteriole constriction GFR ET • (2)renal vessels constriction • RBF sympathetic nerve • Shock RAS • prostaglandin • kallikrein - kinin syetem • ANP • NO
(3) swelling endothelial cell ischemia Na+ - K+ - ATPase free radicalendothelialcellular injury (4)alteration of renal hemorheology fibrinogen Blood viscosity RBC聚集和变形能力 PLT聚集 WBC粘附、嵌顿 微血管改变 renal DIC
②Glomerular lesion filtration surface area Glomerular permselectivity GFR
2Tubular factor • ①tuble obstruction • 管型 阻塞管腔 原尿不易通过 尿量 • 管腔内压 GFR • ②passive backflow • 肾小管上皮细胞变性、坏死 原尿漏出 • 肾间质水肿 囊内压 GFR 尿量
(三)肾细胞损伤及其机制 1、受损细胞的种类及特征 (1) 肾小管细胞 1)坏死性损伤 小管破裂性损伤:可发生于各段肾小管 上皮坏死+基底膜破坏。 肾持续缺血和肾中毒均可见 肾毒性损伤:主要发生于近球小管 仅上皮坏死,基底膜完整。 主要见于肾中毒
2)凋亡性损伤 远端肾小管 (2)内皮细胞 内皮细胞肿胀 血流阻力 内皮细胞受损 PLT聚集,微血栓形成 肾小球内皮窗 GFR 内皮细胞释放舒血管因子
(3)系膜细胞 AngⅡ、ADH 系膜细胞收缩 庆大霉素、腺苷 肾小球血管阻力 滤过面积 GFR
2、细胞损伤机制 (1) ATP合成减少和离子泵失灵 缺氧 缺血 线粒体损伤 ATP 中毒 Na+ - K+ - ATPase Ca2+ - ATPase 细胞内 Na+,H2O 细胞内 Ca2+
(2)自由基(FR) 肾缺血 还原型谷胱甘肽(GSH) FR清除 细胞损伤 再灌注 FR产生 (3)GSH 细胞抗氧化能力 ,膜稳定性 (4)磷酯酶活性 细胞内 Ca2+磷酯酶 A2 细胞膜损伤
(5)细胞骨架结构改变 肾缺血 ATP 细胞骨架结构改变 肾中毒 (6)细胞凋亡的激活
Section 3 Clinical Course and manifestation oliguric ARF 1 oliguria phase(days~weeks) (1)features of urine urine volume:oliguria(400ml/d)or anuria(100ml/d) S.G.:1.010~1.020 Na+ :tubular reabsorption dysfunction urine sediment:erythrocytes, casts, proteinuria
(2) water toxication • oliguria • Catabolism ,内生水 • Transfuse fluid Hypervolemic hyponatremia Fluid retention Cell edema
(3) Hyperkalemiamost serious • Urinary excretion of K+ • Tissue destruction • Metabolic acidosis • Transfuse non-fresh blood, high K+ diet • hyponatremia,exchange of K+and Na+ Movement of K+ from cells into ECF Hyperkalemia
(4) Metabolic acidosisgrogressive,difficult to correct • GFR excretion of acid production • Secretion of H、NH3 , reabsorption of HCO3– • Catabolism , acid production Metabolic acidosis Hyperkalemia
(5) Azotemia(NPN>40 mg/dl) • Excretion of protein metabolite • Protein catabolism 血中尿素、肌酐、尿酸等非蛋白氮 称为氮质血症
2 diuresis phase(1~2W) • Mechanism : • 肾血流量和肾小球滤过功能渐恢复; • 新生的小管上皮细胞浓缩功能低下; • 血中尿素等大量滤出,渗透性利尿; • 肾间质水肿消退,阻塞解除。
manifestation: • polyuria,>400 ml/d; • Early stage: Hyperkalemia, Azotemia , Metabolic acidosis; • Late stage:dehydration, hypokalemia, hyponatremia, infection. 3 recovery phase
Nonoliguric ARF Feaures: • 肾病理损害较轻:尿量不少; 氮质血症 • 肾小管功能障碍:低比重尿; 尿钠低 • 病程短,预后好,但可互相转化。
Section 4 Treatment Principle of ARF 1. Treat the cause; 纠正灌流量不足;慎用肾毒药物; 利尿以解除阻塞;抗感染等 2. Rescue actively. 纠正水电紊乱; 纠正代酸; 处理高钾;控制氮质血症; 透析治疗.
患儿女,11月。因呕吐、腹泻伴发热9天,无尿5天入院。患儿女,11月。因呕吐、腹泻伴发热9天,无尿5天入院。 • 9天前无诱因出现腹泻,每天3~4次,伴频繁呕吐,非喷射状,量较多;同时发热,体温最高41℃。给予口服抗生素治疗,三天后腹泻、呕吐次数减少,但体温仍在38~39℃之间。近5天一直无尿。体检:呼吸60次/分,脉搏120次/分,血压85/54mmHg。昏睡状态。双眼睑及球结膜水肿,睑结膜稍苍白,口唇干裂,咽充血,颈无抵抗;呼吸深大。 • 实验室检查:便常规正常;血钾8.6mmol/L,血钠128mmol/L,氯化物100mmol/L, 血钙1.98mmol/L,血磷2.33mmol/L, 尿素氮37.12mmol/L,血肌酐804.44μmol/L;血气分析:pH7.17, PCO224.5mmHg, HCO3-8.6mmol/L, • SBE -18.3mmol/L;心电图:室内传导阻滞,T波高尖。
Chronic Renal Failure Section 1 Conception etiological factors destruct nephron Dysfunction ofexcretion and endocrine waste product , acid-base and electrolyte disorders, dysfunction ofendocrine
Section 2 Causes of CRF • Renal diseases:chronic glomerulonephritis et al • Vascular disorders:diabetes mellitus、hypertensive disease、Periarteritis nodosa, et al • Urinary tract obstruction:urinary calculus、prostatic hyperplasia et al
Section 3 Clinical Course of CRF • compensatory stage • Renal insufficiency stage • Renal failure stage • Uremia stage
Section 4 Pathogenesis • Intact nephron hypothesis • Glomerular hyperfiltration hypothesis • Trade-off hypothesis • Tubulointerstitial injury
causes Destroy nephron persistently • Intact nephron hypothesis Progressive reduction in the number of nephrons Renal compensation insufficiency Renal failure
Glomerular hyperfiltration hypothesis Compensatory glomerular hyperfiltration Glomerulosclerosis Renal failure
Trade-off hypothesis (矫枉) 浓度正常 GFR↓ 血中某物质(P)↑ (促进排泄) 机体损害 (失衡) 某因子(PTH)↑
血磷恢复 尿磷↑ 磷重吸收↓ (健存肾单位) “矫正” 肾单位↓GFR↓ 磷滤过↓ 血磷↑ 血钙↓ PTH↑ “失衡” 溶骨 骨磷释放 骨钙释放 肾性骨营养不良