Introduction to DMED 525
610 likes | 741 Vues
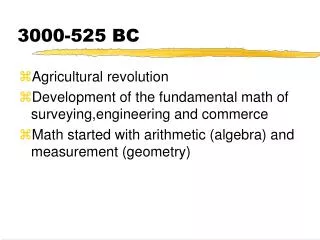
DMED 525, led by Scott North and Andrew Scarfe, is designed to equip medical students with essential knowledge and skills in cancer care over four weeks. The course employs discovery learning, clinical experiences, and workshops focused on building confidence in interacting with cancer patients. Key activities include lectures, standardized patient interactions, and clinical skills training, along with evaluations and exams. Participants will explore cancer diagnosis and treatment, ethics, and the art of breaking bad news, ensuring a comprehensive understanding of oncology essentials.

Introduction to DMED 525
E N D
Presentation Transcript
Introduction to DMED 525 Scott North & Andrew Scarfe Course Coordinators, DMED 525 April 26, 2011
DMED 525 • Welcome • Philosophy of this course • Overview of activities during the next 4 weeks • Discovery Learning • Exam • PCC • Evaluations • Questions
DMED 525 • Philosophy and major objectives: • aim for the level of understanding of a general practitioner • become comfortable with cancer patients • understand general goals of treatment for various situations • develop differential diagnoses to various problems (cancer related or not) • the hidden agenda
DMED 525 • Dentistry students here for first 2 weeks only • DDS 508 has its own coordinator • Dr. Tim McGaw • He is responsible for determining content of your exam, what sessions you are here for and what you will be doing on your own • Med students for 4 weeks
Course Activities • Lectures • Discovery Learning • First hour of session #1 will have a standardized patient (MD students) • Balance of sessions will run like other DL • Consider this an interface between the clinical and preclinical years
Course Activities • Discovery Learning • First hour of the first session of the week will be in Z-L and then you will move to your regular room • 2-3 people will directly interact with SP; others observe and can help if needed • For example, if one or two people are doing the history but someone has a question to ask, feel free to help out • Spend time setting ground rules, etc AFTER you are done with SP and back in regular room • SP’s have to leave
Course Activities • Discovery Learning • These are SP’s so they won’t have physical findings • It’s the process that matters, not necessarily the findings • Abnormalities will be given to you • Practice your techniques • Nobody is grading you on this • Desensitization to the clinical experience
Course Activities • Clinical Experience • Oncology/Hematology/PC clinic • All medical students have the opportunity to sign up for a clinic • May be shadowing or more active depending on other students/residents present • Identify yourself as a second year oncology block student • Contact the preceptor ASAP to make sure they know you’re coming • Clinical Skills (mandatory) • Breast examination for medical students
Course Activities • Questions of the Week (QOW) • MCQ’s outlining an issue related to content currently being discussed • 5 questions will be released at 5pm on each of the first 3 Fridays • Complete over the weekend; answers will be released Monday at 8am • A full description of why the chosen answer is correct will be provided • 15 questions over the course of the block • 15% of the final block mark for all students
Course Activities • Art of Medicine (PCC style content) • Break bad news SP exercise (mandatory) (15%) • Ethics and Oncology • Complementary/Alternative medicine • Bereavement • Body image and the cancer patient • Cultural differences and cancer patients • Integrated into the course; no set time • Check oncology timetable for all activities
Course Activities • Weekly Wrap Up • Friday • No new content • We will use a few powerpoint slides to hit the highlights of the week and the major points of the DL case • If you have questions, contact us • We will reply personally to you • If a major issue arises, it can be incorporated into the review session
ExamMed Students • May 20, 2011 • 2 hour exam; computer completed • Different types of questions • MCQ (20) 50% • Matching (10) • Short Answer (1) 50%
MD Students 15 % Breaking Bad News OSCE 15% QOW 70% Final Exam DDS Students Dr. McGaw will outline Final Block Mark
Course Evaluations • Please do these evaluations- it’s how we make things better • Looking for feedback about: • course content • lecturers • DL • Clinical Experience • utility of clinical skills, special activities (PCC)
Contact Info • Feel free to contact us anytime after lectures, small groups or call/write to me • Not just my lectures but anybody’s lectures • email: • Scott.north@albertahealthservices.ca • Andrew.scarfe@albertahealthservices.ca • Open door policy; first name basis
Introduction to DMED 525An Overview of Cancer Scott North, MD DMED525/DDS508 April 26, 2011
Overview • Cancer: how big is the problem • Terms and Definitions • Diagnosis • Treatment • Newer Horizons • How to think about the cancer patient and generate a differential diagnosis
Cancer • What is cancer? • Neoplasia: new growth • Neoplasm: the actual lump of new tissue • Tumour: swelling • An actual definition of cancer is surprisingly hard to come up with • “a neoplasm of abnormal tissue, the growth of which exceeds and is uncoordinated with normal tissue and persists once the stimulus for its growth is removed
Tumours have 2 major components: • Parenchyma: proliferating neoplastic cells • Stroma: supporting tissue • Parenchyma obviously important but the growth/spread of tumour is dependant on stromal cells. Also Nomenclature of tumours is determined by the parenchymal component. • Treatment strategies are aimed at both components. • Suffic “OMA” refers to benign tumours. • Classified from the organ where they originated: Lipoma: fat cell • Carcinoma: cancers of epithelial originally arising from any of the 3 germ layers of the body. Sarcoma: mesenchymal tumours (connective tissues, blood). Adenocarcinoma: carcinomas that form glandular patterns. Squamous cancers: arising from squamous cells and making keratin.
Areas for intervention • Diagnosis • Earlier diagnosis should theoretically save lives • Mammogram, Pap smear, ?PSA for prostate • Treatment • Better treatment modalities • RT, chemo, small molecules • Prevention • Quit smoking, sunscreens
Benign or malignant? • Differentiation: how much do the parenchymal cells look like their normal counterpart • Benign: well differentiated • Malignant: well to poor • Anaplastic: completely undifferentiated • Hallmarks of cancer • Clonality and Invasion/Metastatic potential
Benign or malignant • Premalignant conditions also exist • Metaplasia: replacement of one normal epithelium with another, but in an unusual location • Reversible • Dysplasia: disordered growth and differentiation of an epithelium • reversible
Benign or malignant • Cancer doesn’t happen overnight • Multiple insults to the cells • Progression through metaplasia, dysplasia and ultimately frank cancer • Further insults that lead to more aggressive behaviour and spread
Four phases:Transformation: malignant change in cellGrowthLocal invasionMets
Metastatic disease • The hallmark of cancer is its ability to spread distantly in the body • Lymphatics: lymph nodes • Hematogenously: via the blood stream • Liver, lung, brain • Anywhere • Once cancer spreads beyond the organ where it started, it is said to be metastatic
Cancer Development • The preceding processes may take years • If inciting cause removed, reversal of the process may occur if early enough (during dysplastic phase) • E.g. quit smoking • All of this occurs at a microscopic level • How do we know? • How can we detect it?
Detecting Cancer • Clinicians have several ways they can detect cancer • Physical examination • Breast lump • Radiology testing • CXR shows a lung mass • Laboratory and special tests • Pap smears, bloodwork
Detecting Cancer • Ability to detect cancer is dependent on having a large enough mass to find • 0.5 -1 cm mass approx. at lower limits of detection by radiology • 1 gram of tissue • This represents 109 cells • Physical examination even less sensitive • Lethal tumour burden is about 1012 cells
Cancer Detection • Consider the growth kinetics • Original transformed cell: 10 microns • 30 doublings to get to 109 cells • 10 more doublings to get to 1012 cells • For most solid tumours, the vast majority of the life cycle of the tumour is completed by the time it’s detected • If we wait for people to have symptoms, many will be too advanced to be cured • Likewise, if a surgeon removes a mass, there may still be cells left behind Never say “I got it all”
Screening • Screening means testing asymptomatic people at risk for an illness to see if they have it • Cancer screening done for several illnesses • Cervix, breast, prostate, colon • Many cancers have no viable screening options
Diagnosis: Since most tumours cant be detected through screening, often they are only found after patients have symptoms Patients may undergo biopsy prior to surgery Surgical excision is often required Pathologist then examines the specimen to determine malignancy or not
Staging and Grading • After diagnosis is made, the cancer is graded and staged • Grade: how aggressive is it • Well differentiated anaplastic • Higher grade = poorer prognosis • Stage: how much cancer is there? • Local, locally advanced (nodes), distantly metastatic • Higher stage = poorer prognosis
StagingTNM System • T= tumour • Reflection of size of tumour and/or depth of penetration through normal structures • N= nodes • Spread to regional lymph nodes of the primary organ • M= metastases • Distant organ involvement • TNM combinations converted to overall stage • I, II, III, IV • E.g. T2N1 breast cancer = overall stage II • IMPORTANT: We don’t expect you to memorize TNM stages for various cancers although you may see them referred to in lectures
Hematological Malignancies • Unique in that ther e isn’t a discrete organ of origin • The progression from dysplasia CIS Frank invasion is absent (no epithelial surface) • Different staging systems • Diiverse group of illnesses • Leukemia (Cancers of the WBC, platelets or RBCs) • Lymphomas (lymphocytes/nodes) • Multiple myeloma (plasma cells)
Adjuvant Treatment • Management of any given cancer usually has a primary modality of treatment • For example, surgery for breast cancer • Any therapy given in conjunction with the primary therapy to improve chances of cure is called adjuvant therapy • Adjuvant therapy could be radiation, drug therapies or both
Adjuvant Therapy • Principle: microscopic disease persists either locally or distantly (micrometastatic) • If no further treatment given, microscopic cells can then grow into macroscopic cancer masses • Often incurable at this point • Deal with remaining disease when there is the smallest tumor burden • Adjuvant therapy added to primary therapy improves the overall cure rates for many cancers, but not all (it’s like an insurance policy)
Metastatic Therapy • Once cancer spreads beyond the organ where it started, it is said to have metastasized • for most solid tumors, the development of distant metastatic disease means no cure is possible • Therapy may be given in the metastatic setting to improve quantity of life, quality of life or both
Cancer Presentation • General Framework: any cancer can cause symptoms from the local tumor, metastatic deposits, or paraneoplastic phenomena • These may coexist in the patient at any time • Cancer patients may also develop symptoms NOT due to their cancer • Don’t always blame the cancer