Respiratory problems in the OB PACU
600 likes | 909 Vues
Respiratory problems in the OB PACU. Tom Archer, MD, MBA Director, OB Anesthesia UCSD Hillcrest August 16, 2012. Vast subject for one hour. Keep it practical and clinical. Keep it focused on OB and PACU. Enough anatomy and pathophysiology to give background and depth.

Respiratory problems in the OB PACU
E N D
Presentation Transcript
Respiratory problems in the OB PACU Tom Archer, MD, MBA Director, OB Anesthesia UCSD Hillcrest August 16, 2012
Vast subject for one hour Keep it practical and clinical. • Keep it focused on OB and PACU. • Enough anatomy and pathophysiology to give background and depth.
What we like from nurses and OBs: • Get us involved early! • We should never be upset with your getting us involved early in patient care! • Morbid obesity • Asthma • Anesthesia fears, Hx of problems • Any significant medical problem
Use simple observation • Talk with and examine the patient. • Don’t think too much about fancy tests.
Signs and symptoms • What is the patient experiencing? Talk to her! Is she cyanotic? Put her on O2! • What is her voice like? • Does sitting up make it better (diaphragm descends, lung expands)? • Can the patient move her arms and legs?
Signs and symptoms • How much air is the patient moving? Put your hand to her mouth. • What do you hear when you ask her to take a rapid, deep breath? • Has she had breathing problems in the past (asthma)? • What does she usually use (rescue inhaler)?
Signs and symptoms • What is the SpO2? Is the sensor applied properly? Same side as BP cuff? • What do you hear on auscultation? • Listen in all lung fields. Anything? Rales, wheezes, stridor?
Signs and symptoms • Rales: too much fluid in the alveoli. • Wheezes: (expiratory sound) narrowed intra-thoracic (bronchial) tubes • Stridor : (inspiratory sound): narrowed extra-thoracic trachea or larynx.
Signs and symptoms • What are the neck veins like? • CXR– essential for any serious problem ABG– nice if you can get it, but don’t waste time and effort if you can’t. Think arterial line for serial ABGs.
What is the patient experiencing? Talk to her! • Don’t forget to talk with the patient! • When did the problem start? • Has this ever happened before? • Does she have chest pain?
Put her on O2! Is she cyanotic? • Cyanosis means there is de-oxygenated blood, blood is not “matched” with O2. • Blood that passes through the lung without getting exposed to oxygen. • “Shunt” or “low V/Q”
www.argentour.com/tangoi.html The dance of pulmonary physiology— Blood and oxygen coming together.
Sometimes the match between blood and oxygen isn’t perfect! http://www.bookmakersltd.com/art/edwards_art/3PrincessFrog.jpg
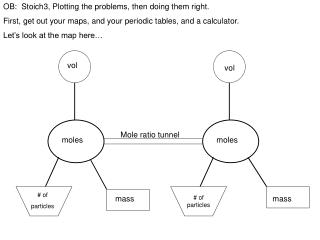
Failures of gas exchange Shunt Low V/Q Alveolar dead space Diffusion barrier alveolus capillary High V/Q
ABGs • In respiratory distress, we expect both PO2 and PCO2 to be decreased. • If PO2 is decreased and PCO2 is increased, this is a true emergency! • Normally, hyperventilated parts of lung will compensate for hypoventilated parts of lung for CO2, but not for O2
Respiratory changes of pregnancy:Mother-to-be is consuming more O2, producing more CO2 and is breathing harder!
Mom 4 ml O2 / kg / min Feto-placental unit 12 ml O2 / kg / min Mother is consuming and delivering oxygen for two! www.studentlife.villanova.edu
At term, mother has respiratory alkalosis with metabolic compensation (less HCO3- buffer). Chestnut
Functional residual capacity (FRC):gas left in the lung after we breathe out.
Functional residual capacity (FRC) is our “air tank” for apnea. www.picture-newsletter.com/scuba-diving/scuba... from Google images
Pregnant Mom has a smaller “air tank”. Non-pregnant woman www.pyramydair.com/blog/images/scuba-web.jpg
Pregnant patient has less “margin of safety” for apnea. • If pregnant patient stops breathing she will desaturate faster than non-pregnant patient. • Apnea from: hypotension, seizure, anesthesia induction, high spinal, magnesium overdose, etc.)
“Ramping up” the obese patient to facilitate intubation. Sitting up will also help any respiratory problem in the PACU. www.airpal.com/ramp.htm
Wheezing • Expiratory sound. • Worse with low lung volumes. • Smooth muscle contraction + airway edema + secretions • Sit patient up / beta agonist rescue inhaler / steroid?
Wheezing is not a complete diagnosis • Smooth muscle spasm (bronchospasm) can cause wheezing. • Airway edema can cause wheezing (fluid overload, CHF)
All That Wheezes Is Not Asthma: Diagnosing the Mimics www.mdchoice.com/emed/main.asp?template=0&pag...
He3 MR showing ventilation defects in a normal subject and in increasingly severe asthmatics. Author Samee, S ; Altes T ; Powers P ; de Lange EE ; Knight-Scott J ; Rakes G Title Imaging the lungs in asthmatic patients by using hyperpolarized helium-3 magnetic resonance: assessment of response to methacholine and exercise challengeJournal Title Journal of Allergy & Clinical ImmunologyVolume 111 Issue 6 Date 2003 Pages: 1205-11
Pulmonary edema www.learningradiology.com/.../cow267lg.jpg
Pulmonary edema is not a complete diagnosis! • Too much water in the lung. • Hydrostatic pressure: heart failure or simple fluid overload. • Alveolar capillary damage and fluid leak: aspiration, sepsis (both lead to ARDS).
Pulmonary edema • Hydrostatic– too much pressure in the alveolar capillaries (normal lung + too much fluid pressure). • Too much IV fluid (pre-eclampsia) • Congestive heart failure (peripartum cardiomyopathy? LV failure with pre-eclampsia?) • Renal failure www.learningradiology.com/.../cow267lg.jpg
Pulmonary edema • Increased capillary permeability (lung damage). • Pre-eclampsia • Aspiration (usually with GA) • Sepsis (chorioamnionitis) • Anaphylaxis (antibiotics) • Pulmonary embolus • Amniotic fluid embolus (very rare) www.learningradiology.com/.../cow267lg.jpg
Atelectasis • An area of lung is compressed. • External compression (obesity, pregnancy, supine posture) • Gas absorption (mucus plug) or after right mainstem bronchus intubation. • Treatment is upright posture, deep breathing and removal of mucus plugs.
Atelectasis– left upper lobe www.med.yale.edu/.../graphics/rad1.gif
Has her voice changed? Does she have stridor? • Voice change– larynx change • Edema from ETT trauma • Edema from pre-eclampsia • Allergic reaction (hereditary angioedema).
The AIRWAY can be closed off by swelling of tongue or larynx.
Normal larynx http://www.dochazenfield.com/images/Larynx_side-by-side_Rotated_Labeled.gif
http://www.healthsystem.virginia.edu/Internet/Anesthesiology-Elective/images/anesth0018.jpghttp://www.healthsystem.virginia.edu/Internet/Anesthesiology-Elective/images/anesth0018.jpg
Stridor • Inspiratory “crow”. Listen with stethoscope over the neck as part of your exam. • Stridor suggests obstruction in the trachea, vocal cords or throat.
Neuromuscular paralysis: can the patient move her arms and legs? Did she recently get a dose of epidural local anesthetic (for post-op pain relief)? Does she have a “high spinal” or epidural? Did she get a GA? Does she have residual neuromuscular blockade?
Can the patient move her arms and legs? Magnesium will exacerbate neuromuscular disease or neuromuscular blocking agents. Does she have unrecognized neuromuscular disease? Myasthenia gravis?
Pulmonary embolus • Can have normal chest x-ray. • Can have pain, or not. • Spiral CT is fancy test of choice. • V/Q scan is not nearly as good a test.
Pulmonary embolus • May be associated with hypotension. • May be associated with distended neck veins.
Pneumothorax • After GA and intubation • Feel for subcutaneous emphysema (air). Rice crispies at base of neck. • Tension pneumothorax would have distended neck veins and hypotension.