Calcium channel blockers
310 likes | 3.1k Vues
Calcium channel blockers. Professor Ian Whyte Hunter Area Toxicology Service. Calcium channel blockers. Phenylalkylamines verapamil Benzothiazepines diltiazem Dihydropyridines nifedipine, felodipine, nimodipine, nicardipine, amlodipine, lercanidipine . Calcium channel blockers.

Calcium channel blockers
E N D
Presentation Transcript
Calcium channel blockers Professor Ian Whyte Hunter Area Toxicology Service
Calcium channel blockers • Phenylalkylamines • verapamil • Benzothiazepines • diltiazem • Dihydropyridines • nifedipine, felodipine, nimodipine, nicardipine, amlodipine, lercanidipine
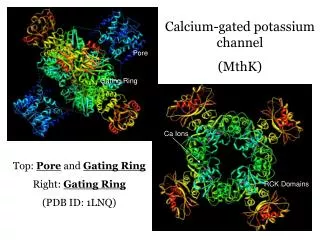
Calcium channel blockers • Block calcium channels (L-type) in heart and blood vessels • prolong depolarisation • ↑QRS width • block SA and AV node conduction • heart block • asystole • vasodilators • cerebral protection
Calcium channel blockers • Hypotension • peripheral vasodilatation and myocardial depression • Bradycardia • AV and SA node block
Antidotes • Correction of acidosis • Calcium loading • Glucagon • Insulin-dextrose euglycaemia • Atropine • Inotropic agents • Cardiac pacing • Bay K 8644 (calcium channel agonist)
Correction of acidosis • Correct acidosis to a pH within the normal range • L calcium channel function is impaired when the pH falls outside the physiological range • acidosis enhances the effect of verapamil and decreases the effect of calcium • sodium bicarbonate significantly improved myocardial contractility and cardiac output in a swine model of verapamil poisoning
Calcium loading • Calcium loading is the most logical and appears to be the most effective agent to use in calcium channel blocker poisoning • It is primarily indicated in patients with heart block (who have usually taken verapamil or diltiazem)
Glucagon • Glucagon is a well-accepted antidote for beta-blocker poisoning • The rationale for its use in CCB poisoning is that it activates myosin kinase independent of calcium flux • Clinical experience suggests it is less effective in this setting than in beta-blocker poisoning
Insulin-dextrose euglycaemia • Insulin infusions should be used to treat hyperglycaemia or hyperkalaemia • Insulin-dextrose euglycaemia is more effective in animal models than calcium, adrenaline or glucagon • Effective in a case series of clinically serious poisonings • Hypotension that is refractory to volume loading, correction of acidosis and calcium salts
Insulin-Euglycaemia • Insulin as an inotrope • myocardial ischaemia/infarction • endotoxic shock • cardiogenic shock post cardiopulmonary bypass • CCB and –blocker induced myocardial depression • Yuan TH, Kerns WP, Tomaszewski CA,Ford MD, Kline JA. Insulin-glucose as adjunctive therapy for severe calcium channel antagonist poisoning. J Tox Clin Tox 1999; 37(4): 463–474
Insulin-Euglycaemia • Rationale • In unstressed, aerobic state the myocardium relies primarily on free fatty acids (FFAs) for mechanical energy • During shock, substrate preference shifts from FFAs to carbohydrate oxidation
Insulin-Euglycaemia • In the presence of • inhibition of insulin release • insulin resistance • poor tissue perfusion • impaired glycolysis and carbohydrate delivery • Systemic hyperglycaemia and inefficient myocardial energy transfer • myocardial depression
Insulin-Euglycaemia • Hypokalaemia • Shift of extracellular K+ to intracellular via Na+/K+ pump • Na+ shift means resting membrane potential becomes more negative (hyperpolarisation) • decrease arrhythmias • Prolongs plateau phase of action potential • increases calcium entry • Aim for K+ 2.8–3.2 • Replace if K+ < 2.5
Atropine • Vagal tone is increase by vomiting and gastrointestinal decontamination • Atropine should be given to all patients who are vomiting or having GI decontamination • Atropine should be given to all patients with bradycardia • A response may only occur after calcium loading
Inotropic agents • Dopamine is the initial pressor agent of choice (75% response) for diltiazem overdose • Isoprenaline produces a therapeutic response in 50% of patients • Action is predominantly through increasing the frequency of impulses originating in the SA node • These agents are often ineffective as chronotropic agents when there is a high degree of conduction block
Cardiac pacing • Ventricular rather than atrial pacing • In severe poisoning the heart may fail to capture and pharmacological therapy will still be required
Calcium channel agonists • Calcium channel agonists (eg. Bay K 8644) would appear to be a logical antidote • Animal studies using these compounds have not been very promising