Perinatal Safety Intervention Program (PSIP): Design and Development
160 likes | 343 Vues
Nancy Lenfestey, MHA, 1 Nancy Chescheir, MD, 2 Margot Schwartz, MPH, 1 Celeste Mayer, PhD, RN 2 , Douglas Kamerow, MD, MPH, 1 . Perinatal Safety Intervention Program (PSIP): Design and Development . AHRQ Annual Meeting September 10, 2012. RTI International

Perinatal Safety Intervention Program (PSIP): Design and Development
E N D
Presentation Transcript
Nancy Lenfestey, MHA,1 Nancy Chescheir, MD,2 Margot Schwartz, MPH,1 Celeste Mayer, PhD, RN2, Douglas Kamerow, MD, MPH,1 Perinatal Safety Intervention Program (PSIP): Design and Development AHRQ Annual Meeting September 10, 2012 RTI International University of North Carolina (UNC) Health Care
Overview • Why focus on perinatal safety? • PSIP pinwheel • Audience • Toolkit background, goals, objectives • Toolkit development and structure • PSIP phases and toolkit testing • Current status and plans
Why Focus on Perinatal Safety? • Birth-associated adverse outcomes: 2-10% (80-400,000 annually), half of which are preventable (Forster et al., 2006, Leape, 2008) • 30-40% of “near misses” and severe maternal morbidities may be preventable through changes in patient, health care provider, and system factors. (Geller, 2007)
Financial Consequences • Approximately 50 percent of hospital risk management budgets are allocated for obstetric events, and birth-related events account for more than 75 percent of claims paid in amounts over $1 million. (Pettker, 2001) • Prevention or minimization of harm through adherence to evidence-based practice guidelines is the best defense against patient harm and malpractice claims. (Cherouny et al., 2005)
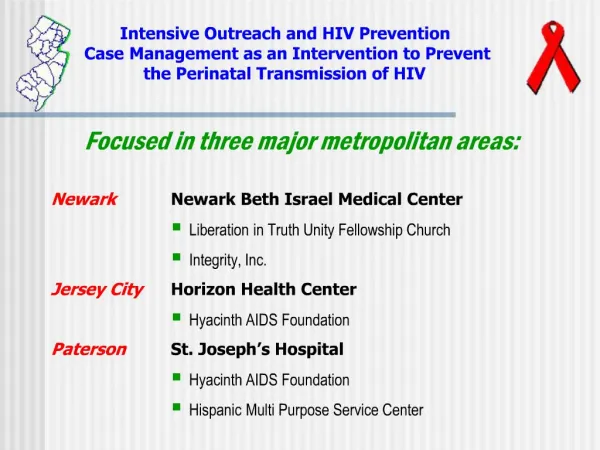
Toolkit: Target Audience • Geared towards perinatal health care teams in the areas of obstetrics, neonatology, and anesthesiology. • Intended for use by perinatal teams across all hospital types, geographic location, and staffing and resource levels. • Toolkit can assist leaders in prioritizing perinatal quality and safety improvement efforts and resource allocation decisions.
Toolkit: Background • Developed under an AHRQ contract that also includes development of a literature review, interviews with providers, and development of a course design guide. • Provides a clinical basis for integrating CUSP and TeamSTEPPS concepts and methodology with current clinical evidence in a high-risk setting. • Customizable to meet organizations’ individual clinical needs and level of staffing and resources available.
Toolkit: Goals and Objectives • Increase standardization of practices and more consistent use of best practices. • Enhance teamwork, communication, and efficiency of perinatal teams, thereby improving perinatal safety outcomes. • Provide tools and resources that will facilitate greater involvement of patients and families in the care process to foster patient-centered care.
Toolkit: Development Process • Bi-weekly in-person UNC-RTI meetings • UNC develops clinical content • RTI has taken the lead in developing the overall PSIP framework and converting the clinical content into toolkit modules complete with guidance and tools • Integrate feedback from 2 Technical Expert Panel Meetings • Integrate feedback from AHRQ • Integrate feedback from field testing
Toolkit: Structure • 7 clinical modules • Postpartum hemorrhage • Umbilical cord prolapse • Safe performance of Cesarean-section • Shoulder dystocia • Induction of labor/augmentation of delivery • The seizing patient • Identification of the hypoxic fetus • 3 non-clinical • Implementation Basics • TeamSTEPPS • Rapid Response Team
Module Contents • Goals and objectives • Information about epidemiology, risk factors, clinical presentations, potential harms, and clinical interventions • Pre- and post-test questions • Simulations • Process and outcome measures • Tools and references (located in the Appendices for each module)
PSIP User Phases Phase I: • Assessment and Planning Phase II: • Implementation Phase III: • Evaluation and Sustainment
Module Topics • 5 modules completed, sent to AHRQ and ready for field testing • Implementation Basics • Postpartum Hemorrhage (PPH) • Umbilical Cord Prolapse • TeamSTEPPS • Obstetric Rapid Response Teams • Remaining Modules • Shoulder dystocia • Induction of labor/augmentation of delivery • The seizing patient • Safe performance of C-section • Identification of hypoxic fetus
Field Testing • To obtain feedback on the toolkit’s feasibility in civilian and military hospitals • UNC Health Care and Womack Army Medical Center • Field testing topics • Overall impressions • Feasibility and appropriateness • Changes needed?
Additional Activity • HRET CUSP videos • PSIP team is working with HRET to produce videos for cord prolapse and PPH • Videos integrate CUSP with PSIP • September 30th completion date