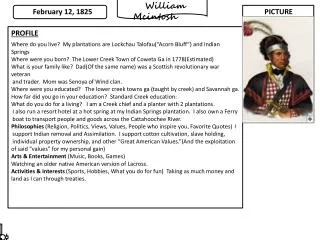
Patient Profile
450 likes | 697 Vues
Patient Profile. 43 year old male corrections officer , and father of two. Exercises regularly in the gym lifting weights. Has been off work on vacation , but has now moved to off work status due to his shoulder pain. Plans to return to work next week on light duty.

Patient Profile
E N D
Presentation Transcript
Patient Profile • 43 year old male corrections officer , and father of two. Exercises regularly in the gym lifting weights. Has been off work on vacation , but has now moved to off work status due to his shoulder pain. Plans to return to work next week on light duty. • Chief complaint: “ I re-tore the labrum in my right shoulder. “ and I don’t see how starting the physical therapy will help. I need an MRI and the insurance won’t due it until I have physical therapy. “ • He is complaining of right sided neck pain with radiation to the medial border of the scapula and right anterior shoulder pain.
Incidence and etiology • Risk Factors for Neck Pain (Childs, et al., 2008) reviewed publications published from 1996 through June 2007 to produce a clinical practice guideline covering risk factors, diagnosis, differential diagnosis, examination and interventions. They concluded that the following were risk factors for neck pain: • age (>40), • psychological health(worrisome attitude) and • poor quality of life (which certainly includes tobacco use). • cycling as regular activity, • less vitality, • a long history of neck pain, • and loss of strength in the hands.
Patient Self Report Inventories • Numeric Pain Rating Scale (NPRS) • Best in the last week: 6/10 • Worst in the last week: 8/10 • Average in the last week: 7/10 • Neck Disability Index (NDI): 45% • Fear Avoidance Belief Scale (FABQ): 32/64 • Physical Activity Subscale: 18/ 24 • Work Subscale : 16/42 • Depression Screen: Negative • During the past month have you been bothered by feeling down, depressed or hopeless? • During the past month have you been bothered by little interest or pleasure in doing things.
Body Chart P1: Anterior shoulder pain, constant, deep ache, sharp with movement 8/10 P2: Right neck pain: Constant deep ache 6/10 P3: Right medial scapula pain: Constant deep ache 4-5/10 X X X X X X X X X X X Relationship of Areas: Worst= P1. P1 P2 P3 Denies numbness and tingling X X
History of Current Episode • Duration of symptoms: 10 days • Mechanism of onset: While on vacation in Hawaii, he was rolled by a wave and hit bottom in a curled position. Neck as stiff and sore immediately and by the next morning, he developed the pain in the anterior shoulder and right scapula. He was able to rest and control activity. When he retuned home he resumed normal weight lifting routine. His shoulder started crunching and cracking, just like it did when he had a previous labral tear. Shoulder neck and scapular pain began to increase when he woke the next morning. • Progression of symptoms since onset: All areas are becoming slowly worse. • Current status (improving, static, worsening): Worsening • Treatment and response: NSAIDS , subacromial injection by MD 3 days ago no help.
Previous History • Previous Episodes: Intermittent stiffness in his neck after heavy lifting or physical interventions on the job, goes away within 1-2 days. Had labral tear 2 years ago related to a forward slide while playing softball. Had surgery and has had no difficulty ever since. • Contributing Factors: None • Previous Treatment: Shoulder surgery on right arm two years ago. • Medical History/Co-morbidities: None
24 Hour Behavior • Night: All areas ache, has difficult time finding comfortable position in which to rest shoulder. Has spent the last two nights in recliner. • A.M.: Better if he can find a comfortable position for the arm. • Day: Varies with use, generally worse by end of day.
Red Flag Screen: Negative • General Health: Excellent • Age 55 with history of cancer: Negative • Cord: Clumsiness in hands, disturbance of gait suggestive of spasticity: Negative • Cauda Equina: Negative • Steroids or anticoagulants: Negative • Numbness and tingling in the hands and feet: Negative • 5 D’s (dizziness, diploplia, dysphagia, dysarthria, drop attacks): Negative
Yellow Flag Screen • FABQ Score: Negative • Depression Inventory: Negative • Behaviors suggestive if depression: Negative • Use of extended rest • Preference for passive treatment • Withdrawal from daily activities • Reports of extremely high pain • Excessive reliance on aids or appliance • Self Medication • I do have some concern about his total commitment to the “torn labrum diagnosis”
Plan of the Objective Examination • Does the nature of the condition or presence of co-morbidities indicate caution?” Yes cervical discogenic with potential radiculopathy, at times severe, moderately irritable • Will you limit the amount of examination? Yes • Will you limit the vigor? : • Examine to P1: Yes • Examine to limit of active range: No • Add overpressure: No • Use repeated movements: Only repeated dorsal glide as potential centralizing technique • Use sustained overpressure, combined movements : No • Are special tests indicated? • Neurological • Wainner TIC • Upper limb tension test • First rib • What structures will you examine on day 1? Cervical spine, screen shoulder
Plan of the Objective Examination • Do you expect the comparable sign to be easy or hard to find? Easy • Why? • Patient report shoulder flexion to reproduce shoulder pain, rotation right to reproduce neck pain. I do not plan to increase vigor to reproduce scapular pain at this time. • What test or movement do you think will reproduce the comparable sign? • Shoulder flexion to reproduce shoulder pain, rotation right to reproduce neck pain. I do not plan to increase vigor to reproduce scapular pain at this time. • Are there contributing factors which must be examined? • Shoulder stability, scapular kinematics • What areas/structures must be cleared (ruled out as contributing factors)? • Visceral disease unlikely given negative history and excellent health.
Objective Examination • Observation • Affect: Clearly uncomfortable and anxious , protective of shoulder • Fitness: Appears fit • Posture • Habitual: Sits fully flexed • Spinal curvature: Forward head,, slight loss of cervical lordosis • Signs of muscle imbalance: scapulae protracted , appears tight in pectorals right trap and right levator. • Functional Screens • Hand behind head: unable due to shoulder pain
Neurological Examination • Reflex: • symmetrical 2+ biceps, brachioradialis, triceps, FDP • LE 2+ • Dermatome: Sensation in tact • Myotome: WNL : Shoulder pain with external rotation and biceps • Hoffman’s: Negative • Upper cervical ligamentous stability • Tectoral Membrane: Negative • Transverse: Negative • Alar: Negative • Cervical Artery Screen: Negative through active movements
Assessment Following the Objective: Review and re-rank your hypotheses
Wainner et al. 2003 • Blinded, prospective diagnostic test study ( 82 patients) to assess the reliability and accuracy of individual clinical examination items and self-report instruments for the clinical diagnosis of cervical radiculopathy • Findings • 34 items had reliability coefficients of at least fair or better. • 13 items had LR above 2 or below .50 • Single test item (TIC)cluster of 4 variables was identified and produced a LR estimate of 30.3 • 95% confidence intervals were wide. • Conclusions: • Many items of clinical examination were found to be reliable and to have acceptable diagnostic properties, but the test item cluster was more useful than any single test item. • ULTT A was most useful for ruling out cervical radiculopathy • Further investigation is required to validate the test item cluster • 11 variables with acceptable diagnostic accuracy
Assessment Following the Objective: Review and re-rank your hypotheses
Assessment Following the Treatment: 1)Review and re-rank your hypotheses2) What is the impact of treatment on the working hypothesis
Assessment Following Treatment • Working hypothesis: • Cervical radiculopathy due to discogenic disturbance C6C7 • Possible shoulder problem not ruled out. Consider patient perspective. • Was you initial hypothesis confirmed, clarified, modified or rejected? • Can the disorder be classified or is a clinical syndrome apparent? • Did your assessment of Presentation change? • Severity: Yes , progressive decrease during treatment • Irritability: Yes , progressive decrease during treatment • Nature : Confirmed with response to treatment • Stage: No still acute • Stability: Improved rapidly, recurrence possible • Did you accomplish what you wanted/needed to do in the first session?? • Yes, more than expected.
Prognosis • Expected level and rate of recovery: Positive response to initial treatment indicates potential for full recovery. Residual shoulder problem is not fully evaluated • Time frame and number of visits: 4-6 over 4 weeks if only the neck is involved • Factors which will promote or impede recovery: In spite of change in symptoms and signs patient remains concerned about labral tear and is insisting on MRO • Likelihood of recurrence: Possible due to the discogenic nature of the problem
Plan for the next session Follow up: Patient cancelled next appointment: Feeling much better, only slight shoulder pain. MRI scheduled. Review of Medical Record: MRI negative