Module Outline
580 likes | 596 Vues
Explore biosafety cabinets, decontamination, and waste management in biohazardous material containment. Learn about risk assessments, containment levels, BSC technologies, and more.

Module Outline
E N D
Presentation Transcript
Biorisk An Engineering Safety ModulePrepared by Valentin MalenkovReviewed by Prof. Marc AucoinSponsored by: MINERVA (www.safetymanagementeducation.com/)and MITACS Chapter 5: Biohazardous Material Containment (Biosafety cabinets, Decontamination/Sterilization, Waste Management Programs)
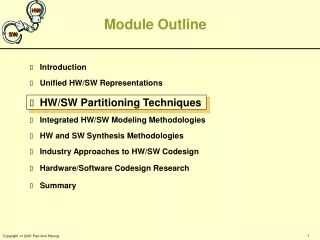
Module Outline Chapter 1: Introduction to Biorisk Chapter 2: Microorganisms, Pathogens, and Toxins Chapter 3: Regulation of Biohazardous Materials and Risk Management Systems Chapter 4: Risk Assessments, Risk Groups, and Containment Levels Chapter 5:Biohazardous Material Containment
Learning Objectives • Understand the measures which need to be taken to achieve effective containment of hazardous material • Gain an understanding of the technologies available for biohazard containment • Develop a working understanding of how a Biological Safety Cabinet operates • Learn the factors which affect decontamination and sterilization requirements • Gain a basic understanding of the various decontamination technologies, their properties, and disadvantages
Containment requirements (recap) • Acts & Regulations • Pathogen/toxin risk groups • Required containment for known pathogens • Risk assessment if not on list • CBSG • Very specific standards • Equipment and SOPs • Risk assessment • Determines what portion of the CBSG to use • Case-specific requirements
Complete Containment • Areas of containment • Physical containment (direct contact) • Air handling • Waste management • Sterilization • Transport • Cradle to the grave approach
Introduction to BSCs • Primary containment device • Used for biohazard handling/experiments • Protect from contamination • Containment level dependant on class • HEPA filtration • “High efficiency particulate air” or “High efficiency particulate arrestance”
Classes of BSCs • 3 main classes • All protect personnel and environment • None recommended for volatile and toxic chemical • Class I • Fume hood with HEPA filter • Negative pressure containment • No protection for biological material • No recirculation • Some use for volatiles • Useable for Risk Group 1, 2, 3 Outside air [Image 1] Contaminated air
Class II Class II, Type A2 • Laminar air flow barrier containment • Re-circulated air barrier • Protects products/materials • Disrupted by movement and obstruction • HEPA filtered exhaust and recirculation • Very sensitive to volatile toxic chemicals Outside air Contaminated air [Image 2] Filtered air
Class II (cont’d) Class II, Type B1 • Four types (A1, A2, B1, B2) • Air intake location/velocity • Varying recirculation ratio • Exhaust type • Useable for Risk Group 1, 2, 3 • Cell culture friendly Outside air Contaminated air [Image 3] Filtered air
Class III • Completely enclosed BCS • Built-in gloves for handling • Replaces positive-pressure suite • Dedicated air handling • Two-stage HEPA filtration • Highly negative pressure • Exhaust out of facility • Designed for Risk Group 4 organisms Pass-through Box Outside air [Image 4] Contaminated air Filtered air
Using BSCs • SOPs may vary with class/type/design • Consult manufacturer documentation • General guidelines in CBSG section 11.4 • When to use BSCs: • Risk Group 2 and above • Aerosols • Vulnerable biological systems (Class II+III) • Cell culture
Using BSCs (cont’d) • When not to use • Toxic fumes • Some exceptions (rated for use, minute amounts) • Open flames • High-velocity aerosols/droplets (Class I+II) • Centrifugation • Shaking • Mixing
Maintaining BSC Containment • Not applicable to Class III • Sash opening only at indicated height • Minimize movement in/around BSC • Avoid side-to-side arm movements • Equipment may create air movement • Air flow in the lab • Air handling changes • Personnel presence/activities • Work one at a time
Maintaining BSC Containment (cont’d) • Distribute work/materials properly • Work as far back in cabinet as possible • Know the “splitting point” • Do not overload with materials • Allow time for air stabilization • On start-up • When loading materials • After aerosol/spill generation • After excessive movement
Testing and Certification • Certification required when: • BSC installed • Any repairs are done • Annual recertification • Conducted by qualified individuals • Approved list from National Sanitation Foundation • Full testing requirements in CBSG (Section 11.3)
Additional Considerations • Ultraviolet light disinfection • Available in most BSCs • Poor primary disinfection method • Cannot penetrate particulates • Deteriorate below disinfection threshold • Not tested regularly • Ergonomics • Use proper posture and support • Avoid continuous use over >1-2hrs
Biosafety and Decontamination/Sterilization • Applies to every stage of bio. hazardous material handling • Materials/consumables • Working surfaces • Facilities and personnel • Regulations/guidelines from various agencies • “Guidelines for the Management of Biomedical Waste in Canada” Canadian Council of Ministers of the Environment • “Handling of Waste Materials in Health Care Facilities and Veterinary Health Care Facilities” Canadian Standards Organization • CBSG (Chapter 16)
Nomenclature • Sterilization: thermal, chemical, or radiological processes for destroying microbial life • Disinfection: Inactivating/removing disease causing organisms • Decontamination: Making surfaces safe to use • Sanitization: Chemical or heat treatment to remove microorganisms from wounds/clothing/surfaces • Cleaning: Water and detergents to remove particulates/spills/soil/etc
Nomenclature (cont’d) • Hazardous waste: all waste requiring special treatment/containment • Can be biological, toxic, radioactive, etc • Regulated based on content • Biomedical waste: waste from human/animal care facilities, human/animal research facilities, clinical and vaccine testing facilities (Canada-wide regulations) • Microbiology waste: cell cultures, stocks, viruses • Sharps waste: needles, syringes, blades, broken glass • Human anatomical waste: tissues, organs, bodily parts (not teeth, nails, or hair) • Human blood and body fluids: all human bodily fluids • Animal waste: tissue, organs, carcasses, bedding, bodily fluids
Decontamination Considerations • Contact time • Long enough to kill/inactivate organisms • Complicating factors • Evaporation rate • Moving parts • Organisms targeted • Varying survivability • Affected by application and location • Surface chemistry • Avoid damaging equipment and surfaces • Safety • Available PPE • Exposure limits
Decontamination Categories • Surface • All working surfaces • Before and after work • Often chemical agent • Ethanol, sodium hydrochloride, etc • Waste/Materials • Anything possibly contaminated • Any material used in BSC • In facility or off-site • Proper labeling • Safe storage (containment) • Proper transportation
Decontamination Categories • Space • Lab/manufacturing areas • Air handling units • Personal • Gowning/de-gowning SOPs • Emergency disinfection equipment/protocols • Spill • SOPs known • Evacuation/signage • Contact info: BSO, management, etc • Required materials on-hand
Chemical Decontamination • Most commonly liquid • Uses: • Flat working surfaces • Equipment • Bottles/containers • Spills • Applicability depends on organisms and contact times
Chemical Decontamination Levels • 3 levels of strength • Based on potency and range of organisms affected • Contact time needed • Prevalence of resistance • Only high level kills highly durable organisms • Can be used for proper starilization • Low • Phenols, quaternary ammonium compounds, chlorhexidine • Kill fungi, some bacteria, and some viruses (enveloped) • Used as sanitizers
Chemical Decontamination Levels • Intermediate • Alcohols, chlorine, iodine • Kill most microorganisms but not spores/mycobacteria • Used as surface disinfectants • High • Formaldehyde, hydrogen peroxide, glutaraldehyde • Can eliminate spores/mycobacteria • Achieve sterility given enough contact time • Efficacy verification • May be required by risk assessment or law • Resistance possible to any chemical/condition • Protocols from Association of Analytical Communities and American Society for Testing and Materials
Autoclave • Thermal decontamination • Heat from high-pressure steam • Can be used to sterilize • Factors affecting efficacy • Time • Temperature • Pressure • Contact with steam • Access to all surfaces • Air displacement must occur
Autoclave cycles • Varies settings for application • Liquid • Slow steam exhaust • Prevents liquid loss (for sterilizing liquids) • Pre-vacuum • Removes trapped air with high pressure • Used for porous materials, rubber, wrapped material • Gravity/Dry • Fast exhaust to boil off liquids, leave material dry • Effluent • Additional decontamination for diverted air/effluent • High containment level facilities
Efficacy testing/Certification • Certification required for use • Biological indicators for CL2+ facilities • Kills live culture to ensure efficacy • Proven inactivation • Chemical indicators for lower CL • Only prove temp. reached • Operating parameters set by application • Determined in risk assessment • Positive and negative controls where required
General guidelines • Never enter autoclave • No flammable materials in or around • Proper PPE at all times • Thermal gloves, face protection, etc. • No manual venting • Allow full venting before opening • Do not overfill containers • No toxins or radioactive materials • Carried out with steam to contaminate facility • Steam penetration required
Hydroclaves • Thermal decontamination with mechanical force • Motor-driven fragmenting arms • Breaks up waste • High temp and pressure • No contact with steam • Full dehydration • ~80% volume and ~50% mass waste reduction • Chemical-free decontamination • Used for sterilization • Kills chemical-resistant micro-organisms (spores, mycobacteria) • High risk of contamination with failed cycle • Waste containers breached • Effluent dumped in drain/regular waste
Hydroclaves Operation • Four-stage process • Loading • Main hatch access (manual or automated) • Sharps, cardboard, bagged waste all acceptable • Sterilization • Mechanical arms break waste and steam jacket heats it • Liquids boil • Sterilization in 20min Adapted from Hydroclave Infectious Waste Solutions website: http://www.hydroclave.com/OURTECHNOLOGY/TheHydroclaveProcess/tabid/82/Default.aspx [Image 6]
Hydroclaves Operation • Dehydration • Waste steam vented through condenser • Sterile waste liquid • Heat and mixing continue until full dehydration • Unloading • Dry waste pushed out unloading door • Mixer rotates to push waste • Sterile, low-volume dry waste • Regular waste disposal Adapted from Hydroclave Infectious Waste Solutions website: http://www.hydroclave.com/OURTECHNOLOGY/TheHydroclaveProcess/tabid/82/Default.aspx [Image 7]
Brief summary of other decontamination technologies. Other Decontamination Methods
Renderers and Biowaste Cookers • Self-contained thermal decomposition units • Renderers • Convert semi-solid waste to paste • Heat and mechanical force • Biowaste Cookers • Sterilize liquid waste with heat • Holding tanks for untreated waste • Homogenous, sterile effluent • Safe for landfill disposal • Little volume reduction • No solid waste/containers
Incinerators • Very high temperature decontamination • Full sterilization • Highly reduced volume/mass for combustibles • Many disadvantages • Viable organisms can be released • Release of toxic/harmful substances • Emission regulations • High space requirements
Irradiation • Electron bombardment for decontamination • Highly lethal to micro-organisms • Short exposure times • Highly specialized equipment • Likely off-site • Requires pre-treatment • Limited penetration depth • Rendering to reduce volume
Microwave • Microwaves used to heat and decontaminate • Temperature up to 950C • ~80% volume reduction • No liquid discharge • Waste pre-treatment required • Water content required • Shredding and moistening
Plasma • Waste passed through ionized gas • Temperatures of 3000-8000oC • Vaporizes waste • Very short exposure times • Highest volume/mass reduction • No pre-treatment/segregation required • Disadvantages • High cost and risk • Effluent gas scrubbed for particulates • Destructive to all materials
Emerging Technologies: Low Temperature Plasma • Non-thermal plasma: electric current passed through gas to create a high energy state • Creates active oxygen species • Radicals (elementary oxygen and ozone) • Damages lipid membranes • Kills bacteria, fungi, and algae • More limited success with spores • Created at atmospheric conditions • Previously only vacuum • No affect on materials decontaminated Korachi M, Aslan N (2013) Low temperature atmospheric plasma for microbial decontamination. Microbial pathogens and strategies for combating them: Science, technology, and education. Ehlbeck J, Schnabel U, Polak M, Winter J, von Woedtke T, Brandenburg R, von dem Hagen T, Weltmann K (2011) Low Temperature Atmospheric Pressure Plasma Sources for Microbial Decontamination. Journal of Physics D Applied Physics 44(1).
Developing the Program • Facility or specific risk assessment • Minimize waste • Contain/decontaminate unavoidable waste • Included in facility (Bio)Safety Manual • Comprehensive SOPs • Identification and segregation • Surfaces and equipment • Consumables and reusable material
Developing the Program (cont’d) • Regulatory requirements • Some federal guidelines • Review Chapter 3 for regulations • More stringent local regulations • Emission and dumping regulations • Adaptable to changing requirements • Changes in waste load and frequency • Potential new protocols/products • Micro-organisms/toxins • Consumables and equipment
Requirements • Waste management plan • Available for personnel • Reviewed regularly • Segregation, packaging, labeling SOPs • Separate biohazards • Colour-code for clarity (various standards) • Red: Human anatomical waste • Orange: All animal waste • Yellow: microbiology waste and waste sharps • Special containment for sharps (puncture-proof) • Controlled storage/holding