Dancing, not wrestling
130 likes | 260 Vues
This resource delves into the nuanced process of helping patients change their behavior. Rather than viewing change as a simple event, it emphasizes understanding the patient's perspective, motivating them to recognize the importance of change, and fostering confidence in their ability to make it happen. Techniques like motivational interviewing, scaling questions, and small, realistic goal-setting are discussed, as well as common pitfalls clinicians may face. By employing a collaborative, empathetic approach, healthcare providers can effectively support patients through their individual change processes.

Dancing, not wrestling
E N D
Presentation Transcript
Dancing, not wrestling How to reach a shared management plan with a patient whom you want to change their behaviour Maggie Eisner, October 2012
Helping people change behaviour - your experience • Think of a patient whom you tried to help to change • What did you try? • What worked? • What didn’t work? • Any ideas about why it worked/didn’t work?
Change • Change isn’t a simple discrete event, it’s a process • Sometimes a crisis can precipitate a sudden change • Change usually involves loss as well as the perceived gain • Stages of Change – precontemplation, contemplation, change
Our role • Traditional advice-giving isn’t useless but absolutely depends on timing • Need to understand the behaviour’s meaning for the patient - how do they see the benefits and problems of the change? • Help patient prepare for change • Encourage to experiment with small steps • Provide information when the patient is receptive • Accept that people have relapses (and help patient accept this too)
Motivational interviewing A video from the USA
Principles • We need to enable the patient to • Believe that change is important • Have confidence in their ability to change • Dancing vs wrestling • Start positive
Tools • The dinner plate, to choose which behaviour to change first • Scaling questions (1-10 scale) • How important is this change to you? • How confident are you that you can change? • Find out – suggest – find out more (Elicit – Provide – Elicit) • What do they know/want to know? • What do they see as their options? • What might their family and friends think? • What do they think? • Help them set realistic goals/targets which they think will work – concentrate on the next small step
Pitfalls (or potholes) Patients • Helplessness • Agree it’s hard, empathise • Help them recall past successes • Resistance • Summarise what they’ve said (instead of getting into an argument) Clinicians • Lecturing • Go back to asking questions about the patient’s point of view • Cheerleading • Bring the focus back to the patient
Go back to the case you talked about • Can you think of how you might have been more effective?
Dance, don’t wrestle … • Help patient believe change is important • Help them get confidence they can change • Start positive • Dinner plate • Scaling questions • Find out – suggest – find out more • Help patient set realistic target – what’s the next small step? • If pt helpless, empathise, remind of past success • If pt resistant, summarise what they’ve said • Stop lecturing and get back to pt’s point of view • Stop cheerleading, get back to pt’s point of view
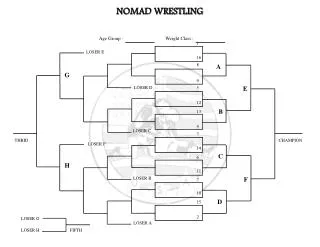
After tea – skills practice • Scenarios for groups of 3 (doctor, patient, observer) – preferably • Mixed ST years • People you don’t know well • Patient – study scenario and get deeply into role • Observer – note specific things the doctor did well or could have done better • Feedback – doctor first (How did you think you did? What did you do well? What do you think you would have liked to do better?), then patient, then observer • Feedback should help the doctor – either affirm what they did well, or specific ideas about what they could do differently (Without specific suggestions, you were really good is as unhelpful as you were rubbish)
Something to think about over tea • Have you ever wanted to change your behaviour? • What helped/hindered you?