CROHN ’s DISEASE
980 likes | 2.25k Vues
CROHN ’s DISEASE. Defini tion Granulomatous inflammatory disease, non specific, producing necrosis and scaring o f segments of gastrointestinal tract, which is chronic and develops in recurring episodes :

CROHN ’s DISEASE
E N D
Presentation Transcript
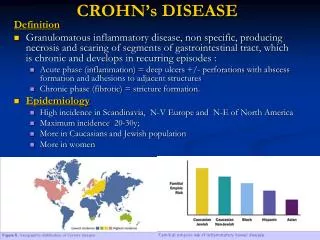
CROHN’s DISEASE Definition • Granulomatous inflammatory disease, non specific, producing necrosis and scaring of segments of gastrointestinal tract, which is chronic and develops in recurring episodes : • Acute phase (inflammation) = deep ulcers +/- perforations with abscess formation and adhesions to adjacent structures • Chronic phase (fibrotic) = stricture formation. • Epidemiology • High incidence in Scandinavia, N-V Europe and N-E of North America • Maximum incidence 20-30y; • More in Caucasians and Jewish population • More in women
CROHN’s DISEASE • Ethiology: • Unknown, probably multifactorial; • Potential factors involved: • Genetic: • Both twins develop disease; • Higher chance for an individual with familial clustering of Crohn’s; • Infectious: • Sugested by the presence of granuloma • There is evidence for: viruses, bacteria and mycobacteria • Concomitent infections – E. coli, Clostridia, Campylobacter. • Alergies: • Alergens in food and inhaled (fungus, molds) – anamnestic data, alergic testing and more favorable results with specific hyposensitisation • Food: • Elimination of weath flour and sugar = evident augmentation
CROHN’s DISEASE • Immunological • Association with: arthritis, eritema nodosum: complex Ag-Ab should be present • Presence of Ab against different Ag structures and increase concentration of IgA; • Inflammatory infiltration and epitheliod granuloma formation = high level immune cell mediated reaction against Ag structures; • Corticoids and immune suppresive medication are highly effected in Crohn’s disease; • Probable: immune changes at the level of the mucosa with hyperactive immune response against foreign Ag with cross reaction and nonspecific tisular injury (innocent bystander)
CROHN’s DISEASE • Pathology: • distribution: • Terminal ileumand colon 90% of cases; • Oro pharinx, esophagus, stomach and duodenum – very rare; • Number of lesions • Numerous lesions with normal segments in between ESSENTIAL of diagnostic
Macroscopy • Edema, eritema, ulcerations, pseudopolyps, fibrosis, sclerosis • Acute phase: bowel • edema, enlarged, inflammed (redish), inert • friabile; • Limits: very clearly delimited • Diseased areas are separated by normal segments ; • Mesentery • Edema, infiltrated with lymph node hypertrophy • Sometimes more extensive then bowel lesions
CROHN’s DISEASE • Presence of ulcer and ulcerations – can be very small or serpent like + transverse ulcers producing the image of islands (cobblestone); • Fissures and ulcers are the origin of fistulas (entero-enteric, entero-colic, entero-cutaneous, entero-vezical, entero-vaginal)
BOALA CROHN • pseudopolyps
Fibrosis, sclerosis, structure formation • Bowel wall very thick (up to 1cm) • Structures, short or long, unic or multiple; • Advanced stages: on long continuous stenosis
CROHN’s DISEASE • Mycroscopy: characteristic = granuloma with epithelioidgiganto cellular cells : • Giant cells + Langerhans cells + limphocytes (+ plasma cells, eosinophils and PMN); • Never caseousnecrosis≠tuberculosis; • Same inflammation in regional lymphnodes • Inflammatory infiltration is found through all strata of the bowel wall;
CROHN’s DISEASE • Symptoms • Insidios onset but mai also be sudden; • A. symptoms associtaed with bowel problems • PAIN • Dull pain, medium intensity in the RLQ • Colicky when associated with obstruction: may be projected in the upper abdomen. • DIARHEA • 4-6/day – watery or semisolid • Proportional to extent of lesions and activity of disease; • Bleeding per rectum: distal lesions. • NAUSEA, VOMITING, BORBORISM. • B. general symptoms • fever 38 0C, +/- chills • Weight loss: diarhhea plus reduced surface for nutrient absorbtion
C. extraintestinal Skin „metastatic” ulcers – submamar, subpubian, abdomen; Parastomal ulceration Anal and perianal ulcerations: eritema nodosum; Aftoid oral ulcerations Pyoderma gangrenosum. Joints Peripheral arthriits Spondilitis ankilopoetica Artralgia. Hepatobiliary Sones due to interruption of enterohepatic cycle; Granulomatous hepatitis; Steatosis ; Cholangitis; Fibrosis. Urinary Stones; Hydronefrosis; Fistula. Ocular Iridociclitis ; keratitis; conjunctivitis; uveitis Hematological anemia; trombocitosis; limfocitosis – B12, ferum, folic. acid deficit CROHN’s DISEASE
Clinical examination general: malnurishes, pale, cutaneous lesions; abdomen: inspection nothing Regional distension (stenosis); P.O. scars – important postapendectomy . palpation Pain in the RLQ Guarding: perforative complications; Palpable bowel loop in RLQ, deep, badly delimited, painful. percution dull ascultation borborism, sometime. perineal region Perianal fistula; ulcerations; fissure. rectal Often nothing; Sometimes diffuse inflammation. Fistula entero-cutaneousvisible; entero-vezical disuria, polakiuria pneumofecaluria. recto-vaginal – symptoms and visible on direct examination. in the gallbladder: similar with acute cholecistitis retroperitoneal – diffuse celulitis (very severe but very rare) CROHN’s DISEASE
CROHN’s DISEASE • Paraclinical • Lab • anemia – most oftem microcytic, hypochromc but macrocytic anemia can develop (B12 deficit) • leucocitosis • In acute phase • in complications (absces, fistula) • trombocitosis • ESR increased; • Electroliteembalance due to diarhea
Radiology - barium meal • Alternation of normal and affected areas • Early stages • nonspecific; • irregular folds, thickened folds; • Ulcers: deep in the wall aspect of rose thorn associating 3 aspects • Pseudopolyps; • Small spiculiform lateral ulcerations • Large ulcers ; IRREGULAR COBLESTONE • Advanced stages • No more folds; • Rigid stenotic tube • Stenosis + distended segments above; • Fistulas. • particular • Terminal ileum – rigid cord; • Cecum – filling defect on the inner border + retraction.
Endoscopy GOLD STANDARD Small lesions + biopsy + extent of lesions + monitor Rectoscopia: 75% normal; Coblestones aspect Ulcers or stenosis friable mucosa that bleeds on touch. Colonoscopy – similar + ileum!!! Gastroscopy
Biopsy • Deep + multiple • Even in normal area. • Others: • Plain abdominal X-ray – in onclusive disease; • Bone X-ray for associated bone disease; • Fistulography. • Laparoscopy
CROHN’s DISEASE Diagnostic: positive • Clinical scenario • Young pt with diarhhea, abdominal pain I RLQ (often) +/- mass on palpation +/- fissure or fistula perianal.. • Radilogy • segmentary, discontinuous lesions and asymetric lesion; • Deep transmural ulcers; • „cobblestone”, „string sign”, presence of pseudopolipilor; • Stenosis and fistula. • Endoscopy • Skip lesions; • Multiple ulcers associated with edematous mucosa +/- stenosis • Pathology • epithelio-giganto-celular granuloma; • lymphocytes and plasma cells infiltration - suggestive
BOALA CROHN Diferential1. Ileal disease • Acute ileitis • Acute apendicitis, apendiceal plastic peritonitis. • tuberculosis • More general signs and PPD+; • Biopsy. • Adnexal tumors. • Ileal carcinoid tumors: carcinoid syndrome • Radiation enteritis • After RXT and diseapears after months. • Cecal tumors – local aspects may be misleading
BOALA CROHN Diferential 2. colonic disease • Ulcerative colitis • Colonic cahnges in laxative abuse • Watery diarrhea in a person that uses laxatives • Rx – loss of haustrations and signs of iritable bowel syndrome. • Ischemic colitis • Diverticulosis • Cancer • Poliposis • IBS
Complications - local • Abscess formation • Fistula • Stenosis • Inflamatory or scars; • Incomplete obstruction • GI Bleeding - mostly from colic origin • Perforation: free perforation with peritonitis is very unusual. • Toxic megacolon – rare but very serious disease • Toxic status + fever + major abdominal pain + bloody and mucus diarrhea + abdominal distension • RX massive distension and destructuring
Complications - general • Extraintestinal may be considered part of the disease or complications if severe • Cutaneous, joints, liver, small vessels (thromboembolic disease, Takayashu disease • Renal • Urinary lithiasisObstructions due to mechanical compression of urethers; • Neuropsyhic: • Sciesures or tetany due to hypoC and hypoMg • Anorexia • Psihosis. • Malabrobtion with consequences on growth. • Amiloidosis (visceral and renal) – after 10 years of evolution • Endocrine: • amenoreea, infertility, late puberty • Small bowel or colonic cancer – after many years
Medical General Bed rest Psihoterapy; Dietary hypercaloric, hperproteic, vitamines (folic, A, D, K, C, B12) and minerals (Ca++, Mg++, K+, Fe++, Zn++); EXCLUDE: Food with many fibers )mostly in pt with stenosis; Milk – intolerance ; Lipids in case of malabsorbtion of lipids. MAJOR situations- TPN Symptomatic Pain therapy Treat diarrhea: codeine phosphat Treat dep on cause: No spices ; No milk - intolerance; Bile salts: interruption of the liver-enteric cycle; Atb - infection Treat electrolytic imbalance. Traet anemia : Fe, B12, folic acid TREATMENT
TREATMENT - pathogenic • ANTIINFLAMMATORY • 5ASA • Salazopirine: better in colonic disease • ANTIBIOTICS • Metronidazol.; • Chinolone • CORTICOIDS - may induce remission • IMMUNE SUPRESSION • Azatioprina (Imuran) – prevention of recurrence; • 6 mercaptopurine • Cyclosporine • Methotrexat • BIOLOGICAL Infliximab (Remicade)
TREATMENT • SURGICAL • Indications • Acute complications • local complications – stenosis, fistula; • Unclear diagnostic. • Limited resection of involved bowel • Enterostomy – end later resection
TREATMENT • A. Crohn ileocolic • Indications: • fistula; • obstruction;; • Percutaneous drainage and resections
TREATMENT • B. Colonic Crohn • Indication • same; • megacolon toxic. • 3 operaţii: • proctocolectomy(abdomino-perineal) with permanent ileostomy; • Total colectomy and ileostomy but rectum in place; • Total colectomy plus ileorectal anastomosis.
TREATMENT • Anal and perianal • Treatment of the abscess and fistula + treatment of Crohns. • If refractory disease n the rectum - proctectomy
TREATMENT • Obstruction • ileon: • Ileon resection; • Ileo-cecal resection • By pass. • colon: • by-pass; • Ileostomy or colostomy.
TREATMENT • Stenosis • rezections • Stricture-plasty
Long term complication • Cancer • High risk for pt with long term Crohns, strictures and scleroiss cholangitis • Colonoscopic monitoring – 2-3 y • Displastic lesions: colectomy
ULCERATIVE COLITIS • Ethiology • unknown • More frequent USA, England, northern countries; • Onset 18-30y • Under 18 very severe; • Over 50 very unusual. • More often in male pt
UC • Genetic factors • Family clustering; • Possible implication of a defect in IgA production • Infection • Numerous germs isolated but not clear; • Atb not very good; • Probably secondary and cause of recurrence . • Enzimatic • Increased synthesis of lizozim – destroys the protective mucus; • Not clear if primary or secundary. • Psihosomatic • Patients are more psichologically vulnerable to conflict; • Emotional problems involved in onset and maintenance of new episodes
Pathology Macroscopy serosa Acute Reddish and glittering; chronic Pale or pale with red spots. Intestinal wall Initially: Distended, thin; Advanced Shortening of the length; Narrow lumen; No haustrations; Thick wall (due to the muscle layer); Fulminant disease Very dilated bowel. Severe Friable, paper-like. mesocolon initially normal. advanced retracted; Large lymph nodes. Sometimes psudopolyps mucosa: Acute: red Small erosions – ulcers (superficial. Not deep); brittle; Continuous lesions Wieschelmann pseudiopolyps subacute: Patches of renewed musosa near the lesions Intense renewal – mucosal bridges and vegetations chronic Wide spread lesions with incomplete healing of the mucosa; Thin mucosa; UC
UC • Particular aspects – affects only the mucosa of the rectum and the colon • First rectum then colon • The lower the segment the more aggressive the disease; • The lesions are continuous;
UC • Microscopy: • Dilation of vessels folllowed by haemmorhage; • limfocites and plasmocites; • Deep glands are full of neutrophils – abcess of the crypts – ulcerations and pseudopolips. • histology: • Granulocyte infiltration is specific • If inflammation spreads to all layers – toxic megacolon.
UC • Clinic • digestive symptoms • diarrhea: • First in 30-50% cases; • Main symptom 4/5; • Feces in a sero-hematic liquid full of puss • 2-3 up to 15-20 stools/day; • Sometimes just blood per anum • Abd pain: • Colicky – left side • characteristic: • tenesmus; • No more pain after a stool is passed. • General • Fever –septic; • Weight loss; • Vomiting; • Tachycardia - depending on amount of lost fluids.
Clinical exam abdomen: inspection: reduction of subcutaneous tissue;bloating - especially supraumbilical - installation may highlight acute toxic dilatation of the colon. percution: timpanism increased in the case of toxic dilatation of the colon; painful; auscultation: multiple air-liquid noises uncomplicated ulcerative colitis tranquility in ulcerative colitis complicated by megacolon. Rectal exam sphincter tone:increased due to pain;decreased in severe forms; rectal wall:rigid;granular mucosa;stricture areas; Mucosa: endoscopyinflammatory exudate in the rectal mucosa, or the presence of blood, mucus, pus;highlights other injuries:cancer, hemorrhoids, abscesses, fistulas, etc.. UC
UC stool: in severe forms, extensive:stools are unformed, with feces floating in a serous fluid, blood mixed with mucus and pus; bulky stools with much blood.in mild forms stool can be formed with blood and mucus;in forms limited to the rectum:stools, wrapped in blood and mucus; emissions of blood and mucus without stool. general: apathy or restlessness, anxiety;palor; dehydration, malnutrition; detection of systemic events:eye;articulation;skin.
UC • Laboratory: • leukocytosis - active phases; • anemia; • hypoalbuminemia; • electrolytes: significant changes only in severe forms; lowering of Na +, K +, Cl-, Mg + +;
UC • Radiology • Simple x-ray or radioscopy • Always first (perforation, incontinence) • Active phase: • No haustrations; • Thick wall; • Cobblestone aspect – psudopolyps; • Distended lumen;
UC Late, advanced stages • mucosal relief is deleted; • haustations disappear completely; • size is reduced; • linear shape; • distensibility is greatly reduced; • angles rounded; • sometimes stenosis; • rigid tube (microcolia).
UC • Endoscopy • Inititial stages: • Red mucosa with vessels visible; • Friable mucosa; • Bleeding is spontaneous and difuse; • Grainy aspect; • Blood, mucus and pus in the lumen; • Florid stages: • Ulcerations that may converge with one-another; • Crypt abscesses; • False membranes. • Late stages: • Atrophy of the mucosa; • Lack of haustrations; • Pseudopolyps; • biopsy: • Exfoliative cytology
UC • CT, MRI
UC Local complications • May appear in acute UC • Perforation • Acute dilation • Massive bleeding (more than 3000 ml in 24 hours • Perianal lessions • Due to chronic disease • Stenosis of the rectum and colon • Pseudopoliposis • Cancer
UC general complications • articular • most frequently; • 5 categories: • Rheumatoid arthritis; • Spondilitis; • Erythema nodosum; • Joint pain; • Acute toxic arteritis • Spondilitis is the only one that can persist after surgery and medical treatment. • ophtalmologic • conjunctivitis;uveitis;iritis;episcleritis;keratitis;retinitis. • cutaneous and mucous: • cutaneous • Erythema nodosum; • pyoderma gangrenosum; • Urticaria, acnea, dermatitis. • mucous – stomatitis; • liver – chronic liver disease and cirrhosis; • Kidney - stones, hidronefrosis
UC • Diferential • Crohn’s disease • Colorectal cancer • Diseneteria • Ischemic colitis • Polyposis • Bacilarry colitis • Irritable bowel syndrome • Diverticulosis • Piles
UC • Treatment • Objectives: • Reduce the time that the patient spends in acute stages of the disease. • Prevent relapses and complications; • A. Treatment of the acute stage • 1. bed rest • 2. food intake • 3-5 days of a colon sparing diet • Small, frequent meals; • No milk • 3. psihotherapy • 4. correct nutritional and hydroelectrolitical imbalances.
5. antiinflammatories and antibiotics • a) salazopirin • b) 5-aminosalicilic acid • c) corticoids and ACTH • d) antibiotics • fever; • sepsis. • e) immunosuppressive treatment • 6-mercaptopurin; • 6-tioguanin; • Azatioprin • Metrotrexate • Ciclosporin