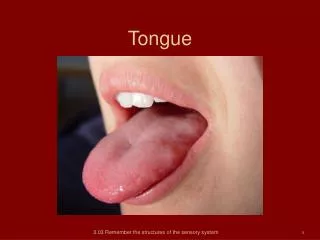
Tongue disorders
470 likes | 1.11k Vues
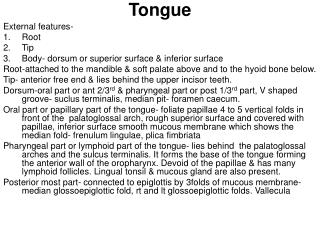
Tongue disorders. Changes in tongue coating. Dr/ Maha Mahmoud Assistant professor, Faculty of Dentistry, Umm Al-Qura University, Makkah, KSA. Tongue coating is formed of:. 1- Tongue papillae. 2- Food debris. 3- Bacteria. 4- Desquamated epithelium. The tongue coating.

Tongue disorders
E N D
Presentation Transcript
Tongue disorders Changes in tongue coating Dr/ Maha Mahmoud Assistant professor, Faculty of Dentistry, Umm Al-Qura University, Makkah, KSA
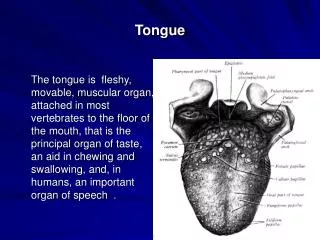
Tongue coating is formed of: 1- Tongue papillae. 2- Food debris. 3- Bacteria. 4- Desquamated epithelium.
The tongue coating varies in different individuals. Varies in the same individual during the day It is continuously formed it is marked in the morning since cleaning factors are at rest. and is removed by: 1- Mechanical factors: speaking and chewing food. 2-Salivary flow
Tongue coating is in a continuous process of removal and formation. If removal exceeds formation atrophy If formation exceeds removal increased tongue coating.
A- Atrophy of tongue coating • The cells forming the filiform papillae and fungiform papillae are of high metabolic activity so any disturbance in enzyme, circulation or nutrients leads to atrophy. • During the process of atrophy: the filiform papillae are affected first, followed by fungiform papillae. • During regeneration: the fungiform papillae regenerate first followed by regeneration of filiform. • Circumvallate and foliate are permanent structures of the tongue coating , don’t participate in atrophy.
1- Deficient or impaired utilization of nutrients 1- Iron deficiency anemia. 2- Pulmonary Vinson syndrome. 3- Pernicious anemia. 4- Anemia associated with parasitic infection as ascaris and bilhariziasis. 5- Malnutrition, malabsorption. 6- Sprue . 7- Chronic alcoholism. 8-Vitamin B deficiency especially (vitamin B2, B6, B12, folic acid and nicotinic acid).
2- Peripheral vascular disease 1- Angiopathy: Diabetes Mellitus. 2-Vasulitis: systemic lupus erythematosus. 3- Endarteritis obliterans: syphilitic glossitis. 4-Obliteration of small blood vessels: scleroderma, submucous fibrosis. 5-Localized vascular insufficiency in elderly patients.
3-Therapeutic agents 1-Drugs that: • Interfere with the growth and maturation of the epithelium e.g cyclosporine. • Induce candidosis e.g. antibiotic, steroid. • Induce xerostomia e.g anticholinergic drugs, radiotherapy.
4- Miscellaneous 1- Frictional irritation: atrophy at tip & lateral borders of tongue. 2- Atrophic lichen planus. 3- Epidermolysis bullosa: ulceration healed by scar. 4- Long standing xerostomia. 5- Diabetes and chronic candidiasis may produce a lesion called central papillary atrophy.
B- Increased tongue coating • The filiform papillae which constitute the keratinizing surface of the tongue are in continuous state of growth and their height is determined by the rate of desquamation process. The later is induced by friction with food, palate and the upper anterior teeth, during eating and speech.
Etiology: • Basically the abnormal increase in tongue coating is due to local environmental changes represented by lack of function and/or changes in the oral flora and these are attributed to: 1- Drugs a- Topical and systemic use of antibiotics. b- Antiseptic mouth washes. c- Oxygen releasing mouth rinse.
Etiology cont… • 2- Febrile illness (general body dehydration, decreased salivary flow, liquid diet and poor oral hygiene). • 3-Stomach upset, vomiting associated with intestinal or pyloric obstruction, debilitated or terminally ill patient. • 4- Mouth breathing
Clinical features: • The increased tongue coating may be stained particularly on the mid dorsum by food, tobacco, drugs or possibly by microorganisms. • In debilitated, dehydrated and terminally ill patients the increased tongue coating may be very thick and has been described as leathery coating.
Treatment • Consist of brushing the dorsal surface of the tongue several times a day systemic antibiotic should not be interrupted but antifungal agent should be used locally. Topical antibiotic and mouth washes should not be used. The condition usually regresses spontaneously when the normal jaw and tongue activity are restored.
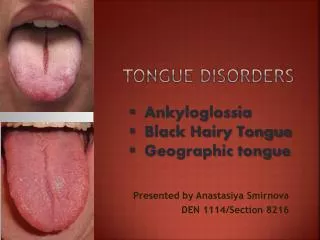
Black hairy tongue • Definition It is a condition characterized by hypertrophy of filiform papillae associated with growth of black pigment producing micro organism.
Etiology 1- Sodium perporate and sodium peroxide mouth wash that stimulate growth of filiform papillae. 2-Topical and systemic antibiotics: ex: penicillin, tetracycline, aureomycin. 3- Systemic disturbance: anemia, hyperacidity, peptic ulcer. 4- Predisposition in some people. Clinical features May be asymptomatic or may cause gagging and tickling.
Management • Removal of the cause • stop t0pical antibiotic. • Brushing of the tongue. • Systemic antibiotic should not be stopped, but antifungal ointment is prescribed in additional to the antibiotic. • Pseudo black hairy tongue means discolouration of tongue by food, smoking and drugs without actual hypertrophy of filiform papillae.
Geographic tongue (benign migratory glossitis (wendering rash)
Site: the dorsum of the tongue. It is an irregularly outlined area, devoid of filiform papillae, with red dots representing fungiform papillae. {occasionally devoid of fungiform}. The margin of the depapillated area is raised with yellowish, whitish tinge. The margin of the lesion shifts as much as ¼ inch per day due to renewed of papillae in one area and loss in another area. It occurs chiefly in children and young adults.
Clinical picture Females are frequently affected more than males. The patient may fell discomfort of pain specially alcoholics and with highly seasoned food. The lesions are usually multiple. Identical lesion is seen in psoriasis and Reiter’s syndrome.
Etiology: Unknown but may be: 1- Associated with fissured tongue (attributed to bacterial irritation). 2-Common in allergic persons (more frequent in atopic patients). 3- Related to psychological factor (the exacerbation has been associated with anxiety and depression. 4-Related to family history (several member of the family may have the disease).
Differential diagnosis Geographic tongue should be differential from 1- Atrophic lichen planus. 2-Fixed drug eruption. The main characteristic features of geographic tongue is the continuous daily migration of the lesion.
Treatment No treatment is indicated as the lesion is self limiting disease. 1- In apprehensive and cancerphobic patient reassurance is required. 2-If the patient is suffering from burning or soreness, benzydamine HCl mouth wash will offer good relief.
Identatoin marking of the tongue Definition: It is crenation marking seen along the tip and lateral margins of the tongue where it rests against the surfaces of the teeth.
Etiology Local factors 1- Tongue pressure habit. 2-Macroglossia (acromegaly, gigantism, etc). 3- Acute inflammation: e.g. erythroma multiform, metallic intoxication, Acute necrotizing ulcerative gingivitis, acute herpetic gingivostomatitis.
Systemic factors 1- Vitamin B complex deficiency. 2-Diabetes mellitus due to decreased muscular tone associated with vitamin B&C deficiency.
Sublingual varices 1- It is formed by enlarged tortuous veins in the sublingual area. 2-It is asymptomatic, but trauma may result in bleeding
Etiology Idiopathic Congential. Found more in elderly people. It may be associated with portal hypertension.
Glossopyrosis Glossodynia Burning tongue painful tongue
Etiology 1- Local factors 2-Systemic factors 3- Psychogenic factors represents 75% of cases.
1- Local factors 1- Irritating calculus, caries, malposed teeth, sharp tooth edge. 2-Electrogalvanic discharge between two dissimilar metals. 3- Oral Candidosis. 4-Dryness of the mouth. 5- Allergic response to lipstick, dentifrices. 6-Excessive smoking. 7- Habit of rubbing the tongue against the teeth. 8-Excessive use of strong mouth wash. 9-Mouth breathing. 10- Highly spicy food.
Erosions on the dorsum of the tongue, caused by very hot food.
2- Systemic factors • Anemia: iron deficiency anemia, pernicious anemia. • Vitamin B complex deficiency. • Chronic alcoholism. • Gonadal deficiency • Diabetes mellitus. • Drugs: fixed drug eruption. • Low serum zinc level. • Tongue tremors e.g. parkinsonism.
3-Psychogenic factors 1- Post menopausal women with cancerphobia. 2- After death of close persons. Psychogenic factors result in glossodynia which is characterized by: 1- No observable clinical cause. 2-Pain does not follow any anatomical distribution. 3- Pain does not interfere with eating or sleeping. 4-Pain intensity increases at the end of the day.
Treatment 1- Removal of the cause if possible. 2-If psychogenic. Reassurance of the patient that there is no malignancy. Valium 5-10 mg t.d.s may be of help. Resistant cases refer to psychiatrist
6- Papillitis (painful foliate and circumvallate papillae) It is the inflammation of foliate and / or the lateral circumvallate papillae. The patient complains of pain at the posterolateral aspect of the tongue. Etiology Sharp distolingual cusp of lower second molar. Sharp edge of a denture. The lesion arises as a result of rubbing or biting the tongue against the teeth, or denture. Digital palpation may reveal a rough or sharp tooth or restoration.
References: • Martin Greenberg and Michel Glick & Jonathan A. Ship. Burkett's Oral Medicine ,Diagnosis & Treatment , 10th ed. 2008, BC Decker, Inc.. • George Laskaris, Pocket Atlas of Oral Diseases, 2nd edition, 2006, Stuttgart , New York.