3 ER Cases
500 likes | 707 Vues
3 ER Cases. Which patient has nerve agent poisoning? 9 year-old with miosis, agitation, copious secretions, uncontrolled urination. HR 120. RR 16/shallow. Sat 83% 15 year-old with generalized seizure, tongue fasciculations, absent gag, absent reflexes

3 ER Cases
E N D
Presentation Transcript
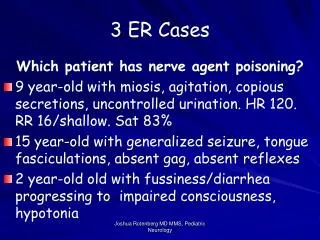
3 ER Cases Which patient has nerve agent poisoning? • 9 year-old with miosis, agitation, copious secretions, uncontrolled urination. HR 120. RR 16/shallow. Sat 83% • 15 year-old with generalized seizure, tongue fasciculations, absent gag, absent reflexes • 2 year-old old with fussiness/diarrhea progressing to impaired consciousness, hypotonia Joshua Rotenberg MD MMS, Pediatric Neurology
Nerve Agents in Children Josh Rotenberg MD MMS Fellow, Pediatric Neurology Staff Pediatrician, WRAMC & NNMC Assistant Professor of Pediatrics, USUHS Joshua Rotenberg MD MMS, Pediatric Neurology
Nerve Agents in Children • Background: Scope of the Problem • Background: The agents • Diagnosis • Isolation/Decon • Treatment • Pediatric Issues Joshua Rotenberg MD MMS, Pediatric Neurology
Background: Scope of the Problem • CWA in US • the most important act of terrorism in which CWA was attempted to use a was the World Trade Center bombing in 1993. • the explosive used by the terrorists contained sufficient cyanide to contaminate the entire structure. • Fortunately, the cyanide was destroyed by the blast Joshua Rotenberg MD MMS, Pediatric Neurology
Background: Scope of the Problem • Police foil terror plot to use sarin gas in London (Filed: 18/02/2001) • Bin Laden British cell planned gas attack on European Parliament (Filed: 16/09/2001) Joshua Rotenberg MD MMS, Pediatric Neurology
Background: Scope of the Problem • Iran-Iraq war (1984-1988) • UN confirmed that Iraq used Tabun and other organophosphorous nerve agents • Sarin and Sulphur mustard used on Kurds in Northern Iraq • Iraq has weaponized VX - 4 tons • Gulf-War: large, urban civil popualation threatened for first time since WW1 Joshua Rotenberg MD MMS, Pediatric Neurology
Sarin Attacks in Japan • Matsumoto Japan, June 1994 • 7 died, 58 admitted, 600 injured • Tokyo Subway March 1995 • Sarin released at several points in the Tokyo subway • 11 killed, 5,500 injured • secondary contamination of the house staff in more than 20% Joshua Rotenberg MD MMS, Pediatric Neurology
Background: The agents • Nerve agents include: • Tabun (GA) • Sarin (GB) • Soman (GD), and • VX Joshua Rotenberg MD MMS, Pediatric Neurology
Background: The agents • Originally developed as insectisides • more powerful than organophosphates • Tabun is easiest and cheapest to manufacture. • Described as a starter agent for CW program. Some consider most likey to be used as terrorist agent. • Sarin has been used in terrorist attacks • VX “only exists in military stockpiles” Joshua Rotenberg MD MMS, Pediatric Neurology
Background: The agents • Exist as a liquid or a gas • Liquid is colorless (g-type) amber-colored (VX) • Gas can be odorless, fruity (tabun) or slight camphor odor (soman) • Vary in volatility – some more persistent than others • Sarin as volatile as water • VX very persistent Joshua Rotenberg MD MMS, Pediatric Neurology
Background: The agents • Toxic effects depend on the concentration of the agent inhaled and the time exposed to the agent. • LD50 - 100 mg/m3 for 1 minute is equivalent to 50 mg/m3 for 2 minutes • Note the vapor density • Sarin 4.86 • VX 9.2 Joshua Rotenberg MD MMS, Pediatric Neurology
When would you launch a sarin attack? Joshua Rotenberg MD MMS, Pediatric Neurology
How do nerve agents work? • Irreversible phosphorylation of cholinesterase enzymes at acetycholine receptors • Nicotinic • Muscarinic • CNS • Adrenal Joshua Rotenberg MD MMS, Pediatric Neurology
Nerve Agents-Mucosal Absorption • Nature and onset of signs and symptoms vary by route of absorption. • Gases may be absorbed through any part of the respiratory tract: mucosa of the nose and mouth to the alveoli of the lungs. • Aerosol particles • > than 5 µm tend to remain in the upper respiratory tract • < than 1 µm tend to be breathed in and out again, although some of these smaller particles may be retained. • They may also be directly absorbed by the eye/skin/GI tract Joshua Rotenberg MD MMS, Pediatric Neurology
Nerve Agents - Absorption via Skin • Agents which penetrate the skin may form temporary reservoirs so that delayed absorption may occur (less so, that OPP). • Even the vapor of some agents can penetrate the intact skin and intoxication may follow. • Wounds/abrasions (even minor injuries caused by shaving ) present areas which are more permeable than intact skin. • The penetration of agents through the GI tract or abrasions may not neccessarily be accompanied by irritation or damage to the surfaces concerned. Joshua Rotenberg MD MMS, Pediatric Neurology
Neuromuscular Effects • Twitching • Weakness • Paralysis • Respiratory failure Joshua Rotenberg MD MMS, Pediatric Neurology
Autonomic Nervous System Effects • Reduced Vision • Small pupil size • Drooling • Sweating • Diarrhea • Nausea • Abdominal pain • Vomiting Joshua Rotenberg MD MMS, Pediatric Neurology
Eyes -- Miosis • most common finding • Matsumoto - 134/219 -2.5 mm or less • improved with atropine • Resolved in a month • Impaired acuity in 124/219 • Blurry vision • Visual Darkness • Ocular pain Joshua Rotenberg MD MMS, Pediatric Neurology
Central Nervous System Effects • Headache • Convulsions • Coma • Respiratory arrest • Confusion • Slurred speech • Depression • Respiratory depression Joshua Rotenberg MD MMS, Pediatric Neurology
Delayed (Chronic) CNS Effects • Giddiness, anxiety, jitteriness, restlessness, emotional lability, excessive dreaming, insomnia, nightmares, headaches, tremor, withdrawal and depression, • drowsiness difficulty concentrating, slowness on recall, confusion, slurred speech, ataxia. • bursts of slow waves of elevated voltage in EEG, especially on hyperventilation, Joshua Rotenberg MD MMS, Pediatric Neurology
Cause of death • In the absence of treatment • anoxia resulting from airway obstruction, weakness of the muscles of respiration and central depression of respiration. • Airway obstruction • due to pharyngeal muscular collapse, • upper airway and bronchial secretions, • bronchial constriction and • occasionally laryngospasm and paralysis of the respiratory muscles. Joshua Rotenberg MD MMS, Pediatric Neurology
Cause of death • With adequate pulmonary support/toilet and atropine, the individual may survive several lethal doses of a nerve agent. • However, if the exposure has been many times the lethal dose, death may occur despite treatment as a result of respiratory arrest and cardiac arrhythmia. • When overwhelming doses of the agent are absorbed quickly, death occurs rapidly without orderly progression of symptoms. Joshua Rotenberg MD MMS, Pediatric Neurology
Other symptoms • Headache • cough • sore throat • Can persist for weeks Joshua Rotenberg MD MMS, Pediatric Neurology
Differential Diagnosis • Sudden Mass casualties - no sign of trauma • Suspect airborne toxin • Hypoxemic, miosis, profuse secretions Anti -Cholinesterase agent • Unconscious, non-hypoxemic Cyanide • venous blood gasses arterialized • Less acute causes of respiratory problems Bo-tox - paralysis, absent reflexes ARDS like picture-anthrax,plague,phosgene Joshua Rotenberg MD MMS, Pediatric Neurology
Diagnosis: • Treatment: institute rapidly based on clinical judgment • Can measure RBC levels of acetycholinesterase • Assess treatment and recovery. • Insensitive as a screen • Matsumoto: ChE decreased in 43% of severely affected • Tokyo: decreased in 74% of admiitted • 4% have genetic low levels • Have genetic high levels, lose 50%, still be nl • One call to lab, 3 send outs-time is critical • Clinical presentation is likely to vary in children. Joshua Rotenberg MD MMS, Pediatric Neurology
Isolation/Decon • Decontamination is necessary • Dogma • 0.05% bleach- people • 0.5% household bleach - equipment • Truth: Use what is available • Good results can be obtained with such widely differing means as talcum powder, flour, soap and water, or special decontaminants. Joshua Rotenberg MD MMS, Pediatric Neurology
Isolation/Decon • Isolation and Decon are necessary in the field • Hot, Warm, Cold Zone - Triage in hot and cold zones • Tokyo: Most casualties arrive in POV • First responders may also be early casualties • Rotate health care workers in “hot zone” • 23 % health care workers had some sort of physical disorder, though mild. • symptoms included ocular pain, headache, sore throat, dyspnea, nausea, dizziness, and nose pain • none was seriously affected Joshua Rotenberg MD MMS, Pediatric Neurology
Triage: Tokyo Subway, St. Lukes • Mild severity • miosis, rhinorrhea, and mild headache • Moderate severity • victims were immobile or complained of moderate degree dyspnea, vomiting, severe headache or with neurologic complication like fasciculation • Critical severity • victims had cardiac or respiratory arrest. Joshua Rotenberg MD MMS, Pediatric Neurology
Treatment • Atropine, respiratory support (secretion management) • Antidotes must be given quickly • But may still be effective if given late, even in extremis Joshua Rotenberg MD MMS, Pediatric Neurology
Treatment • Atropine-give liberally to dry secretions • average total dose in adult 50 mg • Pralidoxime 1 g over 5-10 min • Fasciculations, Seizures treated with benzodiazepines • IM not optimal but acceptable Joshua Rotenberg MD MMS, Pediatric Neurology
Mark 1 - USA/USAF • Atropine - 2 mg (0.7 ml) • 2 PAM Cl autoinjector dispenses 600 mg/2 ml Joshua Rotenberg MD MMS, Pediatric Neurology
Prophylaxis • Pyridostigmine • Military use only Joshua Rotenberg MD MMS, Pediatric Neurology
Supportive therapy for CWA exposure include • Pulmonary treatment/toilet • supplementary oxygen • bronchodilators • Fluids, elctrolytes, nutrition • Hypothermia • Eye care • Attention to skin lesions, • Treatment of complicating infections Joshua Rotenberg MD MMS, Pediatric Neurology
Pediatric considerations/guidance • Antidotes - Dosages • Organ System Specific • Tokyo Subway, 1995 • 16 children • 5 pregnant women • Matsumoto, 1994 • age 3-89 • mean 33 y.o. Joshua Rotenberg MD MMS, Pediatric Neurology
Treatments:Pediatric Dosage • Atropine - ACLS protocol • 0.02 to 0.05 mg/kg to a maximum of 2 mg. May repeat q 10 minutes to reverse cholinergic symptoms. • Min dose – 0.1 mg • Max dose - 0.5 mg child; 1 mg adolescent • Should we be liberal with atropine? • ACLS dosing may not be sufficient Joshua Rotenberg MD MMS, Pediatric Neurology
Atropine Poisoning in Israeli Children • n=268, 92% of pediatric ER’s • Most cases accidental; 7.5% intentional by parents expecting exposure • doses of 0.01 to 0.17 mg/kg • no fatalities,seizures • 0.045 to 0.17 mg/kg - mild effects Joshua Rotenberg MD MMS, Pediatric Neurology
Treatments:Pediatric Dosage • Pralidoxime (US) 2-PAM, Protopam • 20-50 mg/kg x 1 im/iv/sc. May repeat in 1 hour to relieve muscle weakness (nicotinic) • Watch for muscle rigidity, laryngospasm, tachycardia • n.b. others used in Europe and Israel • Some studies suggest continuous infusion may be better • no data in kids Joshua Rotenberg MD MMS, Pediatric Neurology
Treatments:Pediatric Dosage • Diazepam – For severe seizures/status epilepticus • 30d to 5 y – 0.05 to 0.3 mg/kg IV to a max of 5mg/dose. May repeat q15-30 minutes • 5 y.o. – 0.05 to 0.3 mg/kg IV to a max of 10 mg/dose. Joshua Rotenberg MD MMS, Pediatric Neurology
CNS • Carbamate and Organophosphate poisoning in young children -- Pediatric Emerg Care, April 1999 • age 2-8, Median 2.8 • Stupor/Coma 100% • Hypotonia 100% • Miosis 56% • Diarrhea,, Bradycardia, Salivation 25-37% • Pulmonary edema 37% • Predominance of CNS findings in children? • Immaturity of blood brain vs. developmental effect on CNS cholinesterase Joshua Rotenberg MD MMS, Pediatric Neurology
Pulmonary • Increased minute volume and vapor density increases dose of vapor to children • Smaller airway will be more easily obstructed • bronchoconstriction and secretions Joshua Rotenberg MD MMS, Pediatric Neurology
Dermatologic • Skin absorption of liquid may be significant consideration in infants. • Large surface to volume ratio in children compared to adults • Fat soluble agents (less than OPP) • Breaks in skin may permit easier penetration of agent. • Incidence of atopy is approx 4%. Joshua Rotenberg MD MMS, Pediatric Neurology
Dermatologic • Decontamination - Bleach is a mild to moderate mucosal irritant. • 0.5% bleach may cause contact dermatittis • In children can present like “prickly heat”, erythema, edema, blistering. Joshua Rotenberg MD MMS, Pediatric Neurology
Environmental Exposure/ Temperature Regulation: • Hypothermia - Patients will be fully disrobed before decontamination • cold water/bleach solution. • Adequate cover, clothing, diapers should be available for parents and children. • Watch for delayed effects with warming Joshua Rotenberg MD MMS, Pediatric Neurology
Feeding • No information is available regarding breast feeding. • However, nerve agents are less lipid soluble than OPP. • Breast feeding mothers should be encouraged to pump and discard. • Until when? No research done • Institutions should be ready to support infant feedings Joshua Rotenberg MD MMS, Pediatric Neurology
Developmental-Triage and care • Mild and early symptoms may be missed due to a child’s inability to communicate symptoms of pain and pressure. • Alternatively, a physician might dismiss signs symptoms such as sleepiness, hypotonia, cramps, rhinnorhea as typical of other childhood illnesses and behavior. • What will we do with the mother/infant pairs in decon? • Unescorted children? Joshua Rotenberg MD MMS, Pediatric Neurology
Long-Term Effects: • CNS: Organophospate poisoning literature suggests chronic CNS (neurocognitive/cerebellar) and PNS impairment • Carcinogenicity: Limited data in animals suggests no effect. One study suggests genotoxicity in human lymphocytes • Reproductive Effects: Limited data in animals suggests no effect. • Tokyo - well babies Joshua Rotenberg MD MMS, Pediatric Neurology
Take Home Goodies • Mass cas + no trauma=Inhalant • Presentation varies with: • agent, state, absorption, temperature • Autonomic, CNS, muscular symptoms • Start treatment based on suspicion • atropine, respiratory support • Consider diazepam, pralidoxime • Pediatric Issues: acute and chronic Joshua Rotenberg MD MMS, Pediatric Neurology
AAP Guidelines Joshua Rotenberg MD MMS, Pediatric Neurology