Bacillus
610 likes | 3.15k Vues
Bacillus. II MBBS Dr Ekta Chourasia Microbiology. Introduction. Sporing rod shaped bacteria: 2 groups Aerobic – Bacillus Anaerobic – Clostridia Important Bacillus species: Bacillus anthracis Bacillus cereus Bacillus stearothermophilus. Sporing Gram+ve bacilli Bacillus anthracis

Bacillus
E N D
Presentation Transcript
Bacillus II MBBS Dr Ekta Chourasia Microbiology
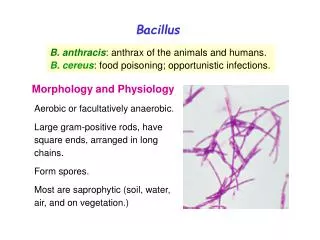
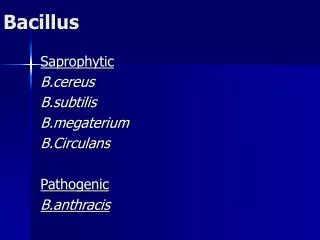
Introduction • Sporing rod shaped bacteria: 2 groups • Aerobic – Bacillus • Anaerobic – Clostridia • Important Bacillus species: • Bacillus anthracis • Bacillus cereus • Bacillus stearothermophilus Dr Ekta Chourasia, Microbiology
Sporing Gram+ve bacilli Bacillus anthracis Anthrax Hide porter’s disease Wool sorter’s disease Malignant pustule Eschar M’fadyean’s reaction Bamboo stick appearance Medusa head colony String of pearl’s reaction PLET medium Ascoli’s test Duckering Anthrax vaccine Bioterrorism Bacillus cereus Gastroenteritis Bacillus stearothermophilus Bacillus: key words Dr Ekta Chourasia, Microbiology
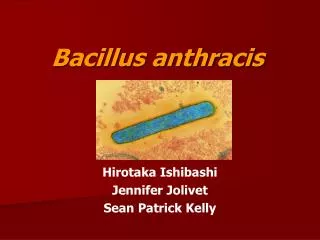
History of Bacillus anthracis • 1st pathogenic bacterium to be seen undermicroscope – Pollender, 1849 • 1st communicable disease shown to be transmitted by inoculation of infected blood – Davaine, 1850 • 1st bacillus to be isolated in pure culture & shown to possess spores – Koch, 1876 • 1st bacterium used for the preparation of an attenuated vaccine – Pasteur, 1881 Dr Ekta Chourasia, Microbiology
Pathogenicity • Anthrax – zoonotic disease primarily involves cattle & sheep. • Animals – infected by ingestion of spores present in the soil • Large no of bacilli are shed in discharges from the mouth, nose & rectum - sporulate in the soil. • Human anthrax – contracted from animals, directly or indirectly. Dr Ekta Chourasia, Microbiology
Pathogenicity: virulence factors Two virulence factors – • Capsular polysaccharide – inhibits phagocytosis, encoded by a plasmid • Anthrax toxin : made up of 3 fractions • Edema factor (EF or Factor I) • Protective antigen factor (PA or Factor II) • Lethal factor (LF or Factor III) * They are not toxic individually, the whole complex produces local edema & generalised shock. Toxin production is plasmid mediated Dr Ekta Chourasia, Microbiology
Human Anthrax • The disease may be • Cutaneous • Pulmonary, or • Intestinal * All types lead to fatal septicemia Dr Ekta Chourasia, Microbiology
1. Cutaneous Anthrax • 95 % of human cases of anthrax • Route of entry: Skin • Sites involved – face, neck, hands, arms & back • Papule Vesicles containing colorless or blood stained fluid Malignant Pustule • ‘Malignant pustule’ – satellite lesions filled with serum or yellow fluid arranged around a central necrotic lesion which is covered by a black eschar • Also known as ‘Hide Porter’s disease’ • Resolves spontaneously, 10-20% of untreaed may develop fatal septicemia or meningitis Dr Ekta Chourasia, Microbiology
2. Pulmonary Anthrax • Alsocalled ‘Wool Sorter’s disease’ – common in workers in wool factories • A life- threatening hemorrhagic pneumonia caused by Inhalation of spores Dr Ekta Chourasia, Microbiology
3. Gastrointestinal Anthrax • Rare • By ingestion of inadequately cooked meat containing B. anthracis spores * Human anthrax can be • Industrial – in meat packing or wool factories • Nonindustrial – frequent association with animals like butchers, veterinarians, farmers Dr Ekta Chourasia, Microbiology
Laboratory Diagnosis • Specimen Fluid or pus from local lesion, blood, sputum • Microscopy • Culture In septicemic anthrax, blood culture should be done • Serological test • Animal inoculation Dr Ekta Chourasia, Microbiology
Microscopy • Large aerobic, non motile, Gm+ve bacilli • Arranged singly, in pairs or in short chains, the entire chain is surrounded by a capsule • Capsules are produced in the presence of bicarbonates or 10-25% CO2 • Spores are oval and centrally located, non bulging • Spores are stained by special stains – Sudan black B. Dr Ekta Chourasia, Microbiology
Microscopic features Staining blood films with polychrome methylene blue: - Pink amorphous material around blue bacillus (M’ Fadyean’sreaction): represents capsular material – used for the presumptive diagnosis of anthrax in animals. Dr Ekta Chourasia, Microbiology
Cultural Characteristics • Grow on blood or nutrient agar, at 37°C • Irregular, round, raised, dull, opaque, greyish white colonies with a frosted glass appearance. • Low power – edge of the colony is composed of long, interlacing chains of bacilli, resembling locks of matted hair – “Medusa Head Appearance” • Gelatin stab culture – “inverted fir tree” appearance, with slow liquefaction starting from top. Dr Ekta Chourasia, Microbiology
Inverted fir tree • Medusa Head Appearance • wavy colonies with small projections
Cultural Characteristics • “String of Pearls reaction” – solid medium containing 0.05-0.5 units of Pn/ ml, in 3-6 hrs the cells become large, spherical and occur in chains on agar surface, resembling a string of pearls. - differentiates B. anthracis from B. cereus • Selective medium – PLET medium – contains polymyxin, lysozyme, EDTA & thallous acetate : to isolate it from mixtures containing other spore bearing bacilli. Dr Ekta Chourasia, Microbiology
Smear from colony Morphology in stained smears from cultures • “Bamboo stick appearance” : bacilli arranged end to end in long chains. Dr Ekta Chourasia, Microbiology
Laboratory Diagnosis • Animal inoculation By rubbing contaminated tissues over shaven skin of a guinea pig • Serology • Ascoli’s thermoprecipitation test –to demonstrate anthrax Ag in tissue extracts • EIA(using purified anthrax toxin Ag) • PCRto detect anthrax contamination of animal & agricultural products Dr Ekta Chourasia, Microbiology
Resistance • Bacilli destroyed at 60°C in 30 mins. • Animal carcasses – bacilli remain viable in BM for a wk & in skin for 2 wks. • Spores – highly resistant, survive in soil for 60 yrs • Spores can be destroyed by • 4% KMnO4 in 15 mins • ‘Duckering’ – using formaldehyde solution for animal products imported into non endemic countries Dr Ekta Chourasia, Microbiology
Duckering • For disinfection of wool – 2% soln of formaldehyde at 30- 40°C for 20 mins • Animal hair & bristles – 0.25% at 60°C for 6 hrs Dr Ekta Chourasia, Microbiology
Prophylaxis • General methods of prevention • Improvement of factory hygiene • Proper sterilisation of animal products • Animal carcasses to be buried deep in quicklime or cremated Dr Ekta Chourasia, Microbiology
Prophylaxis • Active immunisation of • Domestic animals with live attenuated spore vaccines • Persons with occupational risk (butchers, farmers, veterinarians) with a cell- free vaccine containingpurified protective antigen as immunogen. 3 doses IM with annual booster injections. * Anthrax infection in humans give life long permanent immunity & secondary infections are very rare. Dr Ekta Chourasia, Microbiology
Anthrax vaccines • Original anthrax vaccine – developed by Pasteur – live attenuated bacilli vaccine – strain rendered avirulent by the loss of plasmids which encodes anthrax toxin • Live attenuated anthrax spore vaccine • Sterne vaccine – contains spores of a noncapsulated avirulent mutant strain - loss of plasmid which controls capsule production • Mazucchi vaccine – containsspores of stable attenuated Carbazoo strain Dr Ekta Chourasia, Microbiology
Biological warfare • Large epidemics (occasionally) • In 1979 – former Soviet Union: due to accidental release of spores from a military facility engaged in biological research • In 1980s – Zimbabwe: affected 10,000 persons. * Hence the need to develop better human vaccine. Dr Ekta Chourasia, Microbiology
Treatment Bacillus anthracisis sensitive to: - Penicillin - Doxycycline - Ciprofloxacin Dr Ekta Chourasia, Microbiology
Anthracoid bacilli • Belongs to the genus Bacillus • Occasionally cause human infections • Includes B. cereus, B. subtilis, B. licheniformis & other species. • These and a variety of non pathogenic aerobic spore bearing bacilli appear as laboratorycontaminants & resemble anthrax bacilli – Pseudoanthrax or Anthracoid bacilli. Dr Ekta Chourasia, Microbiology
Anthrax bacilli Nonmotile Capsulated Grow in long chains Medusa head colony No growth in Pn agar (10units/ml) Weak or no hemolysis Inverted fir tree growth & slow gelatin liquefaction No growth at 45C Anthracoid bacilli Generally motile Noncapsulated Grow in short chains Not present Grow usually Hemolysis well marked Rapid liquefaction Usually grows Differences b/n Anthrax & Anthracoid bacilli Dr Ekta Chourasia, Microbiology
Bacillus cereus • Readily isolated from soil, vegetables and a wide variety of foods including milk, cereals, spices, poultry & meat. • Causes foodborne gastroenteritis – 2 patterns of disease (diarrhoeal & emetic); both types are mild & self limited, requiring no specific therapy. Dr Ekta Chourasia, Microbiology
Bacillus cereus clinical presentation Gastroenteritis DIARRHOEALFORM EMETIC FORM Incubation period > 6 hours Diarrhoea Lasts 20-36 hours Incubation period < 6 hours Severe vomiting Lasts 8-10 hours
Type I Wide range of foods including cooked meat & vegetables Diarrhoea & abdominal pain develops 8 –16 hrs after consumption Few bacilli seen in fecal specimens Caused by serotypes 2,6,8,9,10 or 12. Enterotoxin resembles LT of E.coli Type II Chinese fried rice exclusively. Acute nausea & vomiting 1-5 hrs after meals, diarrhoea rare Large no of bacilli in cooked rice & fecal samples. Caused by serotypes 1,3 or 5 Toxin resembles staphylococcal enterotoxin Types of Gastroenteritis Dr Ekta Chourasia, Microbiology
Diagnosis • Primarily depends on clinical diagnosis & food sources • Laboratory Diagnosis • Specimen – stool, vomitus, food, blood • Microscopy – not of much help • Culture • Test for toxin – to differentiate from staphylococcal food poisoning. Dr Ekta Chourasia, Microbiology
Culture • Blood agar • Special MYPA medium: Mannitol - egg yolk - phenol red – polymyxin agar : to isolate B.cereus from feces & other sources. Dr Ekta Chourasia, Microbiology
Treatment • Rehydration • Antibiotics – in systemic infections Dr Ekta Chourasia, Microbiology