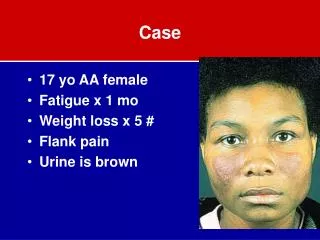
Case
E N D
Presentation Transcript
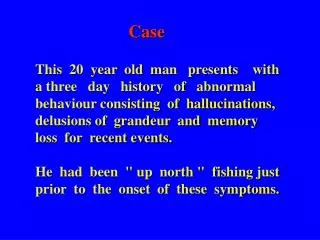
Case • A 46-year-old man with severe vertigo, nausea, and vomiting was brought to the emergency department. She reported that she had felt slightly dizzy when she got out of bed that morning, and that during the next several hours, she had experienced increasing vertigo(illusion in rotation way) and nausea, and eventually vomiting. Her balance was impaired and she was having difficulty focusing her eyes--"everything seems to be jumping back and forth." with vertical displacement of objects. There was no hearing loss or other ear symptoms. Her history was significant only for mild hypertension.
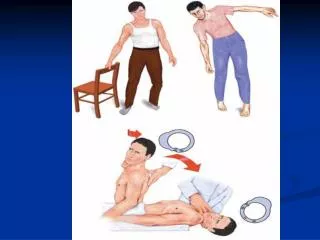
examination • blood pressure was 150/80 mm Hg; her pulse was 88 b.p.m and regular , dehydrated from repeated vomiting. • The patient was able to stand and walk, although she tended to veer to the right and was obviously unsteady. He had a brisk spontaneous nystagmus that was horizontal-torsional ; increased in amplitude when she looked to the left and decreased when she looked to the right, but did not change direction. • Cover-uncover testing indicated the presence of skew deviation, with the right eye slightly lower than the left in all directions of gaze. • The remainder of the physical examination was unremarkable.
دوخة Vertigo , dizzinessversus ataxia= dysequilberium Definition of each and causes? How we can differentiate between them? Concept map of approach ? -type of symptoms and causes? -str . involved=localization -most likely cause -----investigation -Treatments : symptomatic and specific? -
دوخة Vertigo , dizzinessversus ataxia= dysequilberium • 1-Dizziness is non-specific broad term that includes vertigo, pre syncope (lightheadedness, impending fainting or giddiness ,dimming of vision) instability and disequilibrium. Mechanisms? • Vertigo: One of common problem we face in neurology and medicine. • It is illusion of movement of the body or environment .it is often associated with sense of impulsion , visual illusion of movement (oscillopsia), nausea ,vomiting ,or ataxia. • Vertigo must differentiated from non vertiginous dizziness mentioned above that result from impair brain’s supply of blood ,oxygen, or glucose ex: vasovagal ,orthostatic hypotension ,cardiac ischemia and arrhythmias, hypoxia and hypoglycemia ; all may culminate into loss of consciousness and fall. If it is due to decresedcerebral hypo perfusion is called syncope. • don’t forget hyperventilation where dizziness aggravated by 3 min. HV.
2-Ataxia: is incoordination or clumsiness of movement that is not due to weakness. it is caused by vestibular ,cerebellar , or sensory (proprioceptive) disorders. ataxia can affect eye movement limbs, trunk or gait ------------------------------------------------------------------------------- Draw concept map: • When you diagnose vertigo as problem and depending on H., examination &investigation: • 1st step is to differentiate between Central (due to lesion affecting brainstem VN or their connection) versus peripheral v (peripheral vest. lesion affecting labyrinth, inner ear or v. division of 8th cranial nerve). • central is more serious than peripheral • Think about the etiology • Treatment.
Peripheral central • Vertigo: often intermittent :sever often constant usually less sever • Nausea &vomiting : common uncommon • Nystagmus present: never vertical absent if present vertical Unidirectional uni or bi-directional • Hearing loss &tinnitus: often present rarely present • Intrinsic BS signs include : absent typically present -M or S deficit -dysartheria, ataxia • Visual fixation: Inhibited no effect Head thrust sign positive negative • etiology: BPV, V.neuronitis , labyrinthitis VB- ischemia ,MS. cerebellar H .or infarction
Ataxia • is in-coordination or clumsiness of movement that is not due to weakness. it is caused by vestibular ,cerebellar , or sensory (proprioceptive) disorders. ataxia can affect eye movement limbs, trunk or gait. • it result from same central or peripheral lesions that cause V. • Sensory ataxia and motor Ataxias. Vestibular ataxia:nystagmus is frequently present ,usually unilateral most prominent on gaze away from side of lesion, dysartheria does not occur. • It is gravity dependent : in coordination is not present in lying position. • Romberg’s signs is positive.? It is sensory ataxias. Cerebellar ataxia: • cerebellar disease itself or it’s connection. We have limb ataxia (hemisphere lesion) and truncal ataxia (vermis lesion) • frontal lobe lesion may give picture mimic ataxia resulting from controlateral Cerebellar Hemisphere ?due to crossed connection between frontal lobe and cerebellar H.
Cerebellar ataxia: • it characterized by limb or truncal ataxia ,dysartheria ,nystagmus often present with or without other ocular abnormality like gaze paresis and defective saccadic and pursuit movement. vertigo may be present. • The patient is unable to stand with feet together whether eyes is closed or not. • C/F OF cerebellar disease? Specific and non specific. ? Main causes : • *Acquired :infection ,inflammatory , neoplastic and demyelinating ; vitamin E dependent A. • *inherited : Olivopontocerebellar degeneration , Frederich's ataxia. , spinocerebellar degeneration , metabolic like Wilson's disease.
Sensory ataxia? • result from disorder that affect the proprioceptive pathways in peripheral sensory nerve ,sensory root, post. Column of spinal cord or m. lemniscuses. Thalamic and parietal are rare causes of controlateral sensory hemi-ataxia. clinically the patient have: • impaired vibration and position sense, depressed ankle jerk • able to stand with feet together when is opened not if it is closed (Romberg’s sign). • Limb ataxia in legs may present • Vertigo, dysartheria and nystagmus are absent. Main causes: polyneuropathy, posterior SC lesion as in trepanomal disease , MS, Frederich's ataxia
Approach? • history : signs and symptoms vertigo or not , if ataxia which type? • onset &time course • medical H • Family H • general physical examination • neurological examination including: • Mental state • Gait &stance • Cranial nerves checking i.e.: occulomotor,trochlear,abducent and acoustic nerves. • Check for PD which suggest increase ICP, or optic atrophy in case of MS ,neurosyphilis ,B12 deficiency • Facial nerve affection ,corneal reflex associated with C-P angle mass