Case
2.49k likes | 2.68k Vues
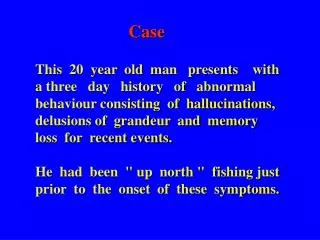
Case. This 20 year old man presents with a three day history of abnormal behaviour consisting of hallucinations, delusions of grandeur and memory loss for recent events. He had been " up north " fishing just prior to the onset of these symptoms. Case.

Case
E N D
Presentation Transcript
Case • This 20 year old man presents with a three day history of abnormal behaviour consisting of hallucinations, delusions of grandeur and memory loss for recent events. • He had been " up north " fishing just prior to the onset of these symptoms.
Case • Physical Exam • Fever 38.0 C • Inattentive • Poor short term memory • Left upper quadrantopsia • Hyperflexia Left upper and lower limb
Case 1 • Where is the lesion? • why? • What is the cause? • What are the immediate treatment priorities?
Herpes Simplex Encephalitis Any time of year, any age, any sex Selective infection of temporal lobes New onset seizures or behaviour disturbance Treat if you suspect - Acyclovir 30 mgm/kg-day
Herpes SimplexTreatment Acyclovir IV Management of ICP (max at 8 – 10 Days) Head up Hyperventilation Mannitol Hypertonic Saline Seizure treatment
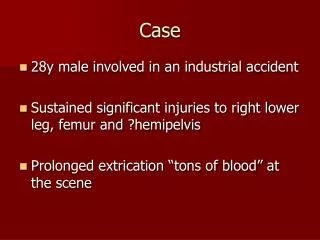
CASE 2 This 24 year old soldier was doing his early morning run with his regimental company. He developed an acute severe headache which caused him to stop and fall to the ground. On examination, he was alert, oriented, moving all four limbs with a normal neurological examination. Where is the lesion ?
CT Scan without contrast
Subarachoid Hemorrhage CT Scan Subarachnoid Blood
Subarachnoid Hemorrhage Worse headache of life Sudden onset, often with activity Signs of meningeal irritation Kernig, Brudzinski Focal signs Signs of coma Positive CT scan Positive LP
Subarachnoid Hemorrhage Blood in subarachnoid space Require urgent referral for angiogram Use acetaminophen not ASA for headache
Subarachnoid HemorrhageInvestigations CT Scan - 90 - 95% sensitive LP - nearly 100% sensitive rbc in CSF xanthochromic in CSF after 12 – 18 hours Angiogram Treatment surgical clipping coiling
Subarachnoid HemorrhageTreatment Clipping Coiling
Headache in the Emergency Room 1. Distinguish ominous from benign headache 2. Treat effectively the benign headaches
Assessment Approach Airway Breathing Circulation Drugs Evaluation Assess, secure Not a problem unless obtunded Assess, assist Not a problem unless obtunded O2 not necessary IV line with crystalloid to restore volume No drugs until diagnosed, unless required to stablize circulation In particular, no analgesics until diagnosed Rapid neurological assessment Investigations as necessary
The Spectrum of Ominous Headaches Subarachnoid hemorrhage meningitis increased intracranial pressure
Danger Signals • the worse headache ever • onset with exertion • decreased level of consciousness • meningeal irritation • abnormal physical signs (including fever) • worsening
All Clear Signals previous identical headaches patient bright and alert neck supple Kernig, Brudzinski’s signs normal examination improving without analgesics
CT Scan detects most conditions causing increased ICP misses 10 - 15 % of subarachnoid hemorrhage misses nearly all cases of meningitis
Modified HIS Diagnostic Criteria for Migraine multiple previous attacks duration of attacks a few hours to a few days headaches have at least two of: hemicranial severe pulsating worse with activity headaches accompanied by at least one of: nausea and or vomiting aversion to light or noise no evidence of ominous disease in history or examination
Classification of Primary Headaches • Migraine • with aura, without aura • Ophthalmoplegic, retinal • Tension Headache • Cluster Headache • Miscellaneous without structural lesion
Treating Migraine in the ER 1. Restore intravascular volume 2. Identify contraindications 3. Choose appropriate medication
Analgesic - Antinauseant Toradol Metoclopramide IV slow push
DHE - Antinauseant Metoclopramide 10 mg IV, followed in 10 minutes by DHE 0.5 - 1.0 mg IV by slow push
Chlorpromazine Ensure patient is normovolemic 250 - 500 cc crystalloid Prepare CPZ for injection 25 mg (1ml) CPZ diluted to 5 ml by adding 4 ml of crystalloid each ml contains 5 mg CPZ Inject into IV tubing 5 mg CPZ every 10 - 15 minutes, stopping when improvement clearly occurring, or 25 mg given Watch for hypotension and sedation
Nasal Sprays • DHE • Sumatriptan
Sumatriptan 1 mg SC if: no ergot or DHE in past 24 hours no contraindication
Patient Instructions:Guidelines Do not drive a car or operate machinery Do not drink alcohol or take tranquillizers, antihistamines, or other drugs that affect the CNS Store in child-resistant containers Neurological followup if frequent or incapacitating
Cluster Headache 1/10 as common as migraine Not genetically determined M:F 6:1 Later Onset Rhythmicity Severe unilateral orbital, supraorbital and/or temporal pain
Cluster Headache Ipspilateral conjunctival injection nasal congestion forehead and facial swelling miosis ptosis eyelid edema Every 2 - 8 times per day
Cluster Headache Trigger alcohol Pathophysiology Role of proximal internal carotid artery Role of histamine Treatment Acute attack ergotamine
Cluster Headache Prophylaxis Sansert Steroids Lithium Calcium channel blockers Combinations
Inflammatory Headaches Most people who think they have sinus headaches usually have migraine or muscle contraction headache Diagnosis requires acute sinusitis Nasal congestion, post nasal drip, fever, pain over the involved sinuses Tender on percussion Sinus xray confirms Treatment Antibiotics or drainage
Temporal Arteritis Progressively obliterative granulomatous arteritis Temporal or occipital Can involve cerebral and ophthalmic arteries 50% will go blind and have a stroke Greater than > years
Temporal Arteritis Usually temporal headache Malaise, anorexia, night sweats, myalgia, +/- fever, jaw claudication ESR > 50 Diagnosis Superficial temporal artery biopsy Treatment Prednisone 60 -100 mgm daily
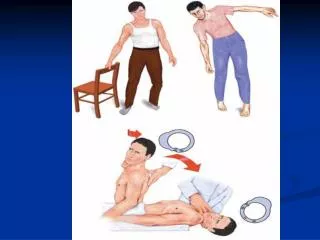
Meningeal Irritiation Meningitis and subarachnoid hemorrhage Occurs due to inflammation and intracranial pain sensitive structures. Subarachnoid hemorrhage - sudden onset meningitis Meningitis - more gradual.
Meningeal Irritiation Occipital and nuchal pain. Interscapular and low back pain. Aggravated by movements Photophobia, vomiting Fever Diagnosis History and physical CT LP
Headache and Brain tumor Traction on intracranial pain sensitive structures. Progressively worsening headache. Morning headaches. Worsen in head down position. Worsen with cough and straining May be localized (constant). Focal neurologic signs.
Benign HeadachesHierarchy of Treatment Acute Treatment Low tech first Prevention Acetaminophen alternate with NSAID Adequate doses and timing according to body weight Avoid codeine
Hierarchy of Prevention Lithium/DBS Valproate/Chlorpromazine Amitriptyline/Beta blockers/pizotyline/Singulair Risk Factors – Headache Diary Alcohol/Foods/Sleep deprivation/Meals/Stress management/Repetitive Stress injury
Hierarchy of Treatment Narcotics/Steroids/Oxygen Triptans/Chlorpromazine Muscle Relaxants/Topiramate/Valproate Acetaminophen/NSAIDS
Case 22 year old man develops double vision especially when looking up or to either side He has noted some increased fatiguability of his muscles EOM shown in video1 Exam otherwise normal
Case He is then given 10 mgm of IV Tensilon (Edrophonium) His extra ocular movements are then reexamined Video 2
Case Where is the lesion? What other tests might be used? What is the commonest treatment? What are the long term risks of the disease?
Myasthenia GravisDefinition * Autoimmune disease with destruction Of neuromuscular junctions * Symptoms - Progressive fatigibility over time
Myasthenia GravisSymptoms * Progressive fatigibility over time * Double vision * Drooping of eyelid(s) * Difficulty swallowing * Change in voice * Difficulty breathing
Myasthenia GravisSigns * Weakness of eyes movements * Weakness of facial muscles * Weakness of swallowing, cough Or gag * Weakness of limbs * No sensory loss