Common Dispensing Errors Experienced in Clinical Settings
610 likes | 1.46k Vues
Common Dispensing Errors Experienced in Clinical Settings. Dr. CHENG Chi Man. Murphy ’ s Law. “ Things will go wrong in any given situation, if you give them a chance. ” (Steps that can go wrong will go wrong). The Person and Systems Approaches to system error.

Common Dispensing Errors Experienced in Clinical Settings
E N D
Presentation Transcript
Common Dispensing Errors Experienced in Clinical Settings Dr. CHENG Chi Man
Murphy’s Law “Things will go wrong in any given situation, if you give them a chance.” (Steps that can go wrong will go wrong)
Reaction to error(The Person Approach) • Poster campaigns • Procedure review • Disciplinary action • Threat of litigation • Retraining • Naming, blaming and shaming
Reaction to error(The Systems Approach) • Error is generalized rather than isolated • System is reviewed to limit the incidence of error • System is reviewed so that if an error occurs its damaging effects are minimized
Human errors cannot be eliminated totally. • Medication errors cause serious consequences.
On 2/5/2007, WHO launched "Nine patient safety solutions" to help reduce the toll of health care-related harm affecting millions of patients worldwide. • Look-alike, sound-alike medication names; • patient identification; • communication during patient hand-overs;
performance of correct procedure at correct body site; • control of concentrated electrolyte solutions; • assuring medication accuracy at transitions in care; • avoiding catheter and tubing misconnections; • single use of injection devices; and • improved hand hygiene to prevent health care-associated infection.
Medical Mishaps occur in all health care settings. • In the United States, it is estimated that 7,000 deaths each year are caused by medication errors. • In Australia, hospitals show that about 1% of all admissions suffered adverse event as a result of medication error.
Medication errors include errors that happen during: • Prescribing • Dispensing • Administering
Dispensing Errors Of 1,000 consecutive claims reported to the Medical Protection Society from 1st July 1996, 193 (19.3%) were associated with medication and prescribing.
Medication errors causes serious consequences to • Patients (physical harm; death) • Doctors (reputation; psychological harm; liability in tort; professional misconduct; criminal liability) • The Medical Profession (trust; relationship between doctors and patients)
Dispensing Right In 2005, the Task Force on Separation of Prescribing from Dispensing was set up by the pharmacists. Recently, the “Separation of Prescribing from Dispensing Alliance (SPDA)” (爭取醫藥分家大聯盟) has been formed by the Pharmaceutical Society of Hong Kong (PSHK), the Practising Pharmacists Association of Hong Kong (PPAHK) and the Society of Hospital Pharmacists of Hong Kong (SHPHK)
WE CAN minimize dispensing errors. • correct attitude • knowing how • doing so • keeping it up
Good DispensingPractice Manual (July 2005)by the Task Force on Drug Dispensingof the Hong Kong Medical Association
The Hong Kong Medical Association CME Bulletin Oct 2006
Prof. David Todd • How to make a diagnosis? • First you need to think of that particular diagnosis.
Alcohol and Bricanyl
“Look-alike” drugs • Look-alike packaging (both bulk bottles and unit-dose packages) Flagyl (metronidazole) Glucophage (metformin)
Delivery from different orders of different medicines / date / companies Errors at delivery team Placement of order for different medicines / dosages at one time Several orders at different date / time Omissions Errors from drug companies Additions RECEIVING Wrong stock checking Wrong placement of order
Different dosages Placing similar drugs together Change to smaller container Placing oral drugs and drugs for external use together Wrong container Similar names Pre-packing Wrong label SHELFING & STORAGE Fancy names Generic names Trade names Expiry date Similar appearances
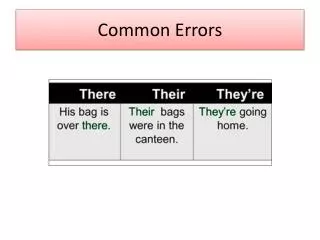
Wrong prescription Mixing up of records Words difficult to read Similar appearances Wrong patient Similar names Wrong record Lack of knowledge TRANSCRIPT- ION Abbreviations Wrong label Wrong dosages Ambiguity
Wrong label Several patients’ medications at one time Wrong quantity Omission Wrong dosages Wrong patients External / internal medicine DISPENSING Wrong strength Wrong instructions Addition
How to prevent dispensing errors? • Removing the hazard • Alerting staff to imminent error • Preventing completion of hazardous action • Minimizing the consequences of error
Removing the hazard (1) • Check medication by doctor after receiving from drug company • Supervise and check by another person when changing from large container to smaller container • Write the name of the medication clearly on all containers
Removing the hazard (2) • Make sure that the labels / lids / covers of the containers will not be mixed up, and check this regularly • Do not give fancy names or similar names to medication • Make sure assistants know both the generic and brand name of each medication, and provide a list where they can confirm
Removing the hazard (3) • Do not order medications which look too similar • Do not put medications which look similar together • Use more individually packed medications
Removing the hazard (4) • Before pre-packing, have another person to check the medication from the large container, make sure that each pack is clearly and correctly labelled. Containers of pre-packed medications should be labelled clearly • Shelf long term medications (esp. dangerous ones: DM, HT, psychotrophic, NSAID) separate with short term medications
Alerting staff to imminent error • Hazard warnings and signs, e.g. Attach tags to containers of medications which are used in daily or BD dosage instead of more frequent dosing • Warning messages in electronic prescribing systems • Warning labels on potentially hazardous drugs, e.g. diabetic medications, potassium, penicillins
We need to pay attention to special patient groups where medication errors can occur more easily • Patients with drug allergy • Patients with chronic illness • Repeat prescription • Children
We need to pay attention to special groups of medicine where medication errors can cause more serious consequences • Medicine with narrow margin of safety • Long term medication • Medications which need dilution or compounding • Medicine for external use only
Certificate Course for Clinic Nurses $960 (6 Sessions) Federation of Medical Societies of Hong Kong Understanding Drug Therapy and Management $6 000 (35 hours) Open University of Hong Kong & Hong Kong Doctors Union 護理人員醫藥基礎認識 $200 (16 hours) Skills Upgrading Scheme, Education and Manpower Bureau 診所醫護人員配藥技巧 $190 (15 hours) Skills Upgrading Scheme, Education and Manpower Bureau Education & Training
Preventing completion of hazardous action Checking and Double Checking
A study of more than 1 million dispensed items in British hospital identified 178 errors (0.018%). The error rate was 0.01% when the dispensing of pharmacists and technicians was double-checked, compared with 0.035% when there was no double-check. Spencer MG. A multicentre study of dispensing errors in British Hospital. Int. J. Pharm Pract 1993; 2: 142-146
The “Swiss Cheese Model” of error prevention The more layers of defence there are and the lower the likelihood of holes in those defences opening up, the lower the risk of a damaging error or accident occurring.
Preventing completion of hazardous action (1) Checking and double checking: • Checked by the one who prepared the medications, then by the doctor, and then by the one who give the medications to the patient
Preventing completion of hazardous action (2) Checking and double checking: • Date • Name of patient • Number of types of medication • Type (make sure all parties can recognise each medication. If in doubt, open a new bottle for confirmation, or contact the drug company)