Managing Common Digestive Problems Through Nutrition
220 likes | 238 Vues
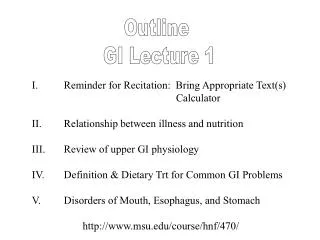
Learn about relationships between illness and nutrition, review upper GI physiology, and define dietary treatments for GI problems such as choking, vomiting, heartburn, ulcers, and more. Understand how to individualize diets for conditions like dysphagia and gastritis. Discover preventive measures and dietary interventions for various digestive disorders.

Managing Common Digestive Problems Through Nutrition
E N D
Presentation Transcript
Outline GI Lecture 1 I. Reminder for Recitation: Bring Appropriate Text(s) Calculator II. Relationship between illness and nutrition III. Review of upper GI physiology IV. Definition & Dietary Trt for Common GI Problems V. Disorders of Mouth, Esophagus, and Stomach http://www.msu.edu/course/hnf/470/
Common Digestive Problems Choking Vomiting Heartburn Ulcers Diarrhea Belching and Gas Constipation
Choking: Food lodges in airway; breathing cut off. Common causes: tough meats, hot dogs, nuts, grapes, carrots, hard candy, etc. Help: Ask if victim can say anything. If not, use Heimlich maneuver. Vomiting: Loss of stomach contents by reverse peristalsis. Massive fluid loss causes electrolyte imbalances, N/V, possible cardiac complications. Restore fluids po or via IV saline/dextrose solution.
Chewing and Swallowing Disorders Cause? Numerous (see Table 21-1) Include dental, medical and surgical conditions. Eating may be difficult and painful, resulting in kcal and protein deficits deteriorating nutritional status Dx and Trt may be prescribed (MD/DO) OR Dietitian’s nutritional assessment may be first to identify.
In All Cases: Individualize the Diet! Whether caused by surgery, mouth ulcers, or low saliva flow Use of mechanical soft diets (excludes foods difficult to chew or swallow) or pureed diets--LONG TERM-- is associated with increased nutritional risk. The Challenges! Minimize nutrient deficiencies Choose foods to enhance appetite Prevent boredom!
Contraindicated Foods Mouth Ulcers: Spicy, acidic or salty foods Foods with nuts or seeds Excessively hot temperatures Reduced Saliva Flow: Savory (salty) snacks that draw moisture from the mouth. Dental hygiene important! Drugs Enhance saliva production Lozenges
What is Dyphagia? Who is at risk? • Disordered or Difficult Swallowing • AGING Stroke patients Neurological Disorders Developmental Disabilities (DD) • Many causes; Often goes undiagnosed • Typical Problem: Repeated Aspiration of Food into the Lungs Aspiration Pneumonia
Dietary Interventions for Dysphagia Standard: Use of mechanical soft diet Good choices: smooth solid foods yogurt puddings custards Baby foods Use commercial thickeners Tube Feedings? Jejunostomy tube safest. Delivery to stomach OK but risk of aspiration is HIGH.
Heartburn/ Indigestion Burning in esophagus cause epigastric pain. Stomach contents reflux into esophagus. Overeating/drinking, smoking, certain medications, Too tight clothing. Remedies: Eat small meals Drink 1 hr before or after meals Don’t lie down after meals Elevate head of bed 4 to 6” Refrain from cigarette smoking
Acid Reflux Disorders Reflux Hiatal Esophagitis hernia Inflammation, scarring due to acid flux into esophagus Protrusion of The stomach thru The Cardiac Sphincter Reduce gastric acidity; Eliminate foods etc. that Weaken cardiac sphincter- Alcohol chocolate garlic Onions Ca Blockers High fat Anticholinergics foods Enteral feeding tubes, Aging, Certain drugs
Ulcers Helicobacter pylori infection Causes Anti-inflammatory medications Excessive gastric acid secretion syndromes
Diet Therapy for Ulcers? Not a major treatment strategy. Current practice: Treat source of infection. Eliminate problem foods. Avoid caffeine- and alcohol- containing beverages ( gastric acid secretions; aggravate existing ulcers)
Gastritis Alcohol Radiation Abuse Therapy Metabolic Stress Food Bacterial Infection Poisoning Acute Transition Trt: Withhold food 1-2 days Liquid diet Bland Diet Colas, Cocoa Bland diet? Avoid irritating foods Caffeine Coffee, Tea Alcohol Decaf coffee or tea Pepper/ spicy foods
Gastric Bacterial Surgery Infection Liver Disease Idiopathic Gastritis Chronic Appropriate Medical Trt + Bland Diet Long-term effects of gastritis: Vitamin B12 deficiency (2˚ to Intrinsic Factor) Perforation Ulcers Malnutrition Esophagitis
Nutritional Complications of GI Surgeries What puts them at nutritional risk? Early satiety Postsurgical or epigastric pain Fear of dumping sx Weight Loss, Serum Proteins (Total Gastrectomies, Jejunostomies= Protein AND Fat Malabsorption) Significant Resection of Gastric Mucosa = Loss of IF production Risk of B12 deficiency
Nutritional Complications of GI Surgeries Malabsorption of: Folate Macrocytic Anemia Iron Microcytic Anemia Fat Malabsorption: Osteomalacia Vitamin D absorption (soft bone disease) (2˚ Ca absorption)
Postgastrectomy Diet Transition from liquids to solids gradually: Limit simple sugars Frequent small meals Liquids in small amts 45 min < > eating. Prevent Dumping Syndrome!!
Diarrhea Loose, watery stools caused by fluid moving too quickly into GI tract for absorption to occur. Replace fluids po or IV
Constipation Defecation with discomfort, pain, or difficulty. Causes: Lack of physical activity Low levels of dietary fiber Inadequate water intake With physician: laxatives enemas mineral oil