Determinants of Islet Remodeling in Diabetic Baboons: Insights from Pancreatic Amyloidosis and Cell Dynamics
250 likes | 269 Vues
This study investigates the correlation between islet remodeling in diabetic baboons and factors such as pancreatic islet amyloidosis, beta-cell apoptosis, and alpha-cell proliferation. By analyzing amyloid deposits, endocrine cell volume, and metabolic parameters in baboons, the study sheds light on the impact of these determinants on islet function and relative cell volume. The findings reveal a significant association between amyloid depositions, insulin resistance, and glucose metabolism in baboons, highlighting the importance of understanding these factors in diabetic pathophysiology.

Determinants of Islet Remodeling in Diabetic Baboons: Insights from Pancreatic Amyloidosis and Cell Dynamics
E N D
Presentation Transcript
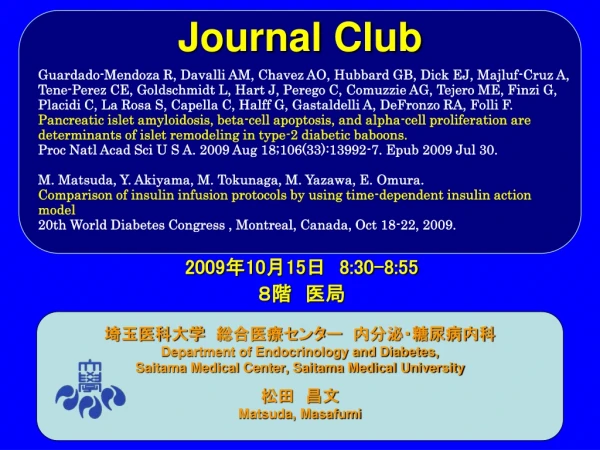
Journal Club Guardado-Mendoza R, Davalli AM, Chavez AO, Hubbard GB, Dick EJ, Majluf-Cruz A, Tene-Perez CE, Goldschmidt L, Hart J, Perego C, Comuzzie AG, Tejero ME, Finzi G, Placidi C, La Rosa S, Capella C, Halff G, Gastaldelli A, DeFronzo RA, Folli F. Pancreatic islet amyloidosis, beta-cell apoptosis, and alpha-cell proliferation are determinants of islet remodeling in type-2 diabeticbaboons. Proc Natl Acad Sci U S A. 2009 Aug 18;106(33):13992-7. Epub 2009 Jul 30. M. Matsuda, Y. Akiyama, M. Tokunaga, M. Yazawa, E. Omura. Comparison of insulin infusion protocols by using time-dependent insulin action model 20th World Diabetes Congress , Montreal, Canada, Oct 18-22, 2009. 埼玉医科大学 総合医療センター 内分泌・糖尿病内科 Department of Endocrinology and Diabetes, Saitama Medical Center, Saitama Medical University 松田 昌文 Matsuda, Masafumi 2009年10月15日 8:30-8:55 8階 医局
2型糖尿病患者の食事に対するインスリンとグルカゴンの反応2型糖尿病患者の食事に対するインスリンとグルカゴンの反応 2型糖尿病(n=12)* 非糖尿病(n=11) 360 330 食事 300 血糖値 (mg/dL) 270 240 110 80 150 インスリン反応の抑制/遅延 120 90 インスリン (µU/ml) 60 30 0 140 130 120 グルカゴン (µµg/ml) グルカゴンの過剰分泌 110 100 90 –60 0 60 120 180 240 時間(分) *5例の患者についてインスリン測定を行った。 Müller WA et al N Engl J Med 1970;283:109–115.より改変
250 4 200 3 150 2 100 1 50 0 血糖がちょっと高めの段階から膵β細胞量は低下している 124 autopsies 剖検例の解析 p<0.001 空腹時血糖 FPG (mg/dl) p<0.01 正常血糖 血糖上昇 糖尿病 膵臓β細胞量 ß-cell Volume (%) p<0.01 p<0.001 正常血糖 血糖上昇 糖尿病 Butler et al, Diabetes 52:102-110,2003
4 3 2 1 0 血糖がちょっと高めの段階から膵β細胞量は低下している 124 autopsies 剖検例の解析 膵臓β細胞量 ß-cell Volume (%) p<0.01 p<0.001 正常血糖 血糖上昇 糖尿病 Butler et al, Diabetes 52:102-110,2003
糖尿病で膵β細胞量が著減 手術例の解析 2 p:NS 膵臓β細胞量 ß-cell Volume (%) 1 p<0.001 0 正常血糖 血糖上昇 糖尿病 33 patients with chronic pancreatitis (n = 17), benign pancreatic adenomas (n = 13), and tumors of the ampulla of Vater (n = 3) Meier JJ et al: Diabetes 58:1595–1603, 2009
40 30 20 10 0 <240 <280 <320 <360 <400 >400 糖尿病 IGTの段階から膵β細胞機能は低下している Lean Gastaldelli, Ferrannini, Abdul-Ghani, DeFronzo, Diabetologia 41:31-39, 2004; JCEM 90:493-500, 2005; Diabetes 55:1430-35, 2006 膵β細胞機能 ∆ INS/ ∆ GLU ÷IR Obese 2-Hour PG(mg/dl) <140 <120 <100 <200 <160 <180 正常血糖 耐糖能異常
GLP-1はヒト膵島細胞の形態を維持した(In Vitro) コントロール GLP-1処置細胞 GLP-1を添加して培養した膵島では、長期間その形態が維持された Day 1 Day 3 GLP-1 islet insulincontent insulin secretion apoptosis caspase-3 activity Day 5 Adapted from Farilla L et al Endocrinology 2003;144:5149–5158.
Background and Aim b-Cell dysfunction is an important factor in the development of hyperglycemia of type-2 diabetes mellitus, and pancreatic islet amyloidosis (IA) has been postulated to be one of the main contributors to impaired insulin secretion. The aim of this study was to evaluate the correlation of IA with parameters and its effect on islets of Langerhans remodeling and relative endocrine-cell volume in baboons.
Method We sequenced the amylin peptide, determined the fibrillogenic propensities, and evaluated pancreatic histology, clinical and biochemical characteristics, and endocrine cell proliferation and apoptosis in 150 baboons with different metabolic status.
Fig. 1. b-Cell function and insulin resistance correlated with amyloid deposits and FPG in baboons. Ln(HOMA-B) (A and B) and Ln(HOMA-IR) (C and D) are depicted according to amyloid severity (IA) and FPG concentration in baboons. (E) Effect of increasing FPG concentration and worsening severity of amyloid deposition on b-cell function (ln HOMA B) in baboons. *, P<0.05 vs. Group 1; †, P< 0.05 vs. Group 1 and 2; ‡, P<0.05 vs. Groups 1, 2 and 3; **, P<0.05 vs. all groups.
Fig. 2. FPG are associated to amyloid deposits, glucagon, and insulin resistance in the adipose tissue, and increases progressively during time in baboons with more severe IA. Relationship between FPG and (A) relative amyloid volume/pancreas; (B) relative amyloid area; (C) islet area free of amyloid; (D) glucose levels during the last 4 years of baboon’s life according to the degree of amyloid severity at death (open circles Group 1, open diamonds Group 2, filled diamonds Group 3, open squares Group 4, and filled squares Group 5); (E) Glucagon levels; and (F) Adipose tissue insulin resistance index (fasting FFA × FPI). *, P < 0.05 vs. Group 1 and 2; **, P < 0.05 vs. G1, 2, and 3; †, P < 0.05 vs. all groups; #, P < 0.05 vs. glucose 1 year before death (in the same amyloid group); ‡, P < 0.05 vs. glucose 3 years before death (in the same amyloid group). (G–L) Congo red staining (40_) in pancreas of baboons with different levels of FPG and IA (FPG for G = 76, H = 80, I = 109, J = 199, K = 195, L = 255 mg/dL). (Bar = 50 mm.)
Fig. 2. FPG are associated to amyloid deposits, glucagon, and insulin resistance in the adipose tissue, and increases progressively during time in baboons with more severe IA. Relationship between FPG and (A) relative amyloid volume/pancreas; (B) relative amyloid area; (C) islet area free of amyloid; (D) glucose levels during the last 4 years of baboon’s life according to the degree of amyloid severity at death (open circles Group 1, open diamonds Group 2, filled diamonds Group 3, open squares Group 4, and filled squares Group 5); (E) Glucagon levels; and (F) Adipose tissue insulin resistance index (fasting FFA × FPI). *, P < 0.05 vs. Group 1 and 2; **, P < 0.05 vs. G1, 2, and 3; †, P < 0.05 vs. all groups; #, P < 0.05 vs. glucose 1 year before death (in the same amyloid group); ‡, P < 0.05 vs. glucose 3 years before death (in the same amyloid group). (G–L) Congo red staining (40_) in pancreas of baboons with different levels of FPG and IA (FPG for G = 76, H = 80, I = 109, J = 199, K = 195, L = 255 mg/dL). (Bar = 50 mm.)
Fig. 3. IA severity is associated to b-cell apoptosis and a-cell proliferation. Percentage of endocrine islet cells in proliferation (Ki67) (A), apoptosis (M30) (B), the difference between these 2 (C), and the proliferation /apoptosis ratio (D) according to amyloid severity. *P < 0.05 vs. control group. Double-label immuno-histochemical stains in 3 baboon pancreases with >50% of IA and hyperglycemia show that nuclear immunoreactivity of the proliferative marker Ki67 does colocalize with glucagon in some a cells (arrow in E; I, andM), but not with insulin in _ cells (F, J, and N). Conversely, cytoplasmic immunoreactivity for the apoptotic marker M30, which detects the caspase cleavage product of cytokeratin 18, does not colocalize with glucagon (G, K, and O), but it does with insulin (arrows in H and L; P). Ki67 and M30 are stained in brown, while hormones are stained in red. Triple immunofluorescence staining (I and J) with Ki67 (green), insulin (red), and glucagon (blue) confirming that nuclear staining of the proliferative marker Ki67 was detected in few glucagon-positive cells (blue, arrows), but not in insulin-positive _ cells (red). A particular at higher magnification (2_) is shown. *, Amyloid deposits autofluorescence. (Scale bar, 10 mm.)
Results Amylin sequence in the baboon was 92% similar to humans and showed superimposable fibrillogenic propensities. IA severity correlated with fasting plasma glucose (FPG) (r = 0.662, P < 0.001) and HbA1c (r = 0.726, P < 0.001), as well as with free fatty acid, glucagon values, decreased homeostasis model assessment (HOMA) insulin resistance, and HOMA-B. IA severity was associated with a decreased relative b-cell volume, and increased relative a-cell volume and hyperglucagonemia. The most important determinants of IA were age and FPG (R2 = 0.519, P < 0.0001), and different FPG levels were sensitive and specific to predict IA severity.
Conclusion These results strongly support the concept that IA and b-cell apoptosis in concert with a-cell proliferation and hypertrophy are key determinants of islets of Langerhans ‘‘dysfunctional remodeling’’ and hyperglycemia in the baboon, a nonhuman primate model of type-2 diabetes mellitus. Finally, a predictive model for islet amyloid severity was generated with age and FPG as required variables.
Message マントヒヒの研究は実際にヒトでできないことができる。 2型糖尿病では膵臓のβ細胞が疲弊しα細胞が増加する。つまり膵臓が時間が経過するに従い変化し滅びる!!! 悪化には時間とFPG(肝臓のインスリン抵抗性が強く影響)が大きなファクター
9:00-10:00 on Wednesday 21/10/2009 14:30-15:00 on Thursday 22/10/2009 Hall 220EInsulin therapy and devices P-1441 Comparison of insulin infusion protocols by using time-dependent insulin action model M. Matsuda, Y. Akiyama, M. Tokunaga, M. Yazawa, E. Omura. Saitama Med Univ. Saitama Med Center, Dept of Endocrinology and Diabetes, Kawagoe-shi, Japan.
Abstract Aims Insulin infusion has been recommended to use in critically ill patients at an in-patients setting to obtain reasonable plasma glucose concentration. However there are many protocols for insulin infusion. It is difficult to compare insulin infusion protocols, because you cannot re-try in the same setting. We have recorded insulin and glucose infusion rate, and plasma glucose concentration during insulin infusion procedures, and applied this time dependent change to a mathematic model which was expressed insulin action by time-dependent two parameters. Using this model, we virtually applied insulin infusion protocols to compare the effectiveness and safety of such protocols. Methods The model was expressed by an insulin-dose dependent line which was determine by insulin resistance index (IRI-abs: how many units of insulin per hour is necessary to keep plasma glucose conc.) an insulin sensitivity index (ISI-del: decline of plasma glucose conc. by infusion of one unit insulin per hour). The relation was plotted on a graph (X: insulin infusion rate, Y: delta PG) and ISI-del and IRI-abs which are time-dependent variables) were identified. Glucose infusion was assessed by the distribution of glucose space, and converted to the difference of PG which is approximated in addition to Y. Mathematically this is written as Y = - (ISI-del(t)) x (X - IRI-abs(t)). Next estimated PG = Current PG + Y. By using this model, Yale Univ. protocol, Braithwaite method, and Davidson's method were compared. Results Data from 50 cases (subjects) (age: M/F = 25/25, age = 54 ± 12 y.o., BMI = 24 ± 5 kg/m2) were re-analyzed. Total time under reconstructed and deconvolution was 3,000 hours. Averages PG were 95, 110, and 97 individually. Frequency of hypoglycemia lower than 50mg/dl of PG were 5, 12 and 8 times individually. In the manual procedure of actual intervention, average PG was 113mg/dl, and frequency of hypoglycemia was twice. Conclusion In the protocols analyzed, Yale Univ. protocol was most effective and safe. Despite of its complicated protocol, it may be a choice to use Yale Univ. protocol. Although there is a limitation, it also may possible to apply a procedure by obverting graphic change of insulin action. Thus manual intervention by obverting graphic change of insulin action would be an alternative choice, and further validation would be conducted.
Message 松田先生はIDFで来週いませんのでよろしく!