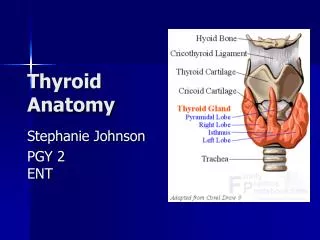
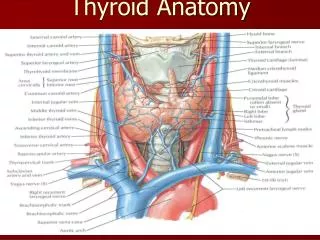
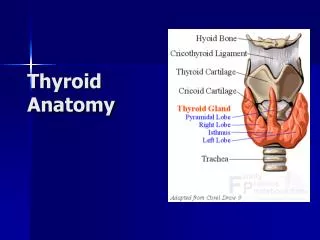
Anatomy of Thyroid
730 likes | 1.38k Vues
Thyroid disease Libo Li MD Department of General Surgery Sir Run Run Shaw Hospital School of medicine, Zhejiang University. Anatomy of Thyroid. Anatomy of Thyroid. Thyroid disease. Nontoxic goiter Hyperthyroidism Thyroid Cancer Thyroiditis. Nontoxic Goiter.

Anatomy of Thyroid
E N D
Presentation Transcript
Thyroid diseaseLibo Li MDDepartment of General SurgerySir Run Run Shaw HospitalSchool of medicine, Zhejiang University
Thyroid disease • Nontoxic goiter • Hyperthyroidism • Thyroid Cancer • Thyroiditis
Nontoxic Goiter • Goiter from the French (goitre) and Latin (guttur), both meaning throat • Defined as an enlargement of the thyroid gland • Endemic when it involves more than 10% of the population • The majority, secondary to iodine deficiency • Especially found in high mountain regions
Nontoxic GoiterClinical thinking • Whether the patient has local symptoms • Whether the goiter is toxic or nontoxic • Whether any of the nodules harbor a cancer • The number and bilaterality of the nodules • TSH level, differential diagnosis of hypothyroidism or hyperthyroidism • Appropriate treatment options for each particular patient
Nontoxic GoiterTaking history • Asymptomatic neck mass • A cough, shortness of breath, stridor, or hoarseness • Choking or aspiration, dysphagia, or pain • Symptoms of hyperthyroidism • Whether the patient has cosmetic concerns • From iodine deficiency region
Nontoxic GoiterPhysical examination • Whether the goiter is confined to the neck • Whether it has a substernal component • Whether tracheal deviation is present • The size and consistency of the goiter • The mobility of the vocal cords by either indirect or direct laryngoscopy
Nontoxic Goiter • Ultrasound • How many nodules? • Bilateral? • Ultrasound characteristics
Nontoxic Goiter • CT scan • Neck and chest, especially substernal thyroid • Rare intrathoracic or aberrant thyroid
Nontoxic Goiter • Fine needle aspiration (FNA) • Suspicious malignent goiter
Nontoxic GoiterTreatment • Iodine diet replacement (endemic goitor) • Surgical resection • Symptoms • Local compression • Secondary hyperthyroidisim • Any suspicious or malignant lesion • Cosmetic reasons • Radioiodine therapy, high risk of pts • Thyroid hormone suppression (not for sporadic goiter)
Sporadic Nontoxic Goiter • Asymptomatic • Euthyroid • Most bilaterally • No efficiency of thyroid hormone replacement • High recurrence postoperatively 30%~40%
Nontoxic GoiterHistory of Thyroid Surgery • First thyroidectomy, in Paris in 1791 by Pierre-Joseph Desault • Antisepsis, hemostasis, and general anesthesia in the 1840s • thyroid surgery became safe • Theodore Kocher, a Nobel Prize in 1909 • From Bern, Switzerland • His pioneering efforts in thyroid surgery
Clinical Statistics • Graves Disease is the most common cause of hyperthyroidism (60-80%) of all cases • Females are affected more frequently than men 10:1.5 • Monozygotic twins show 50% concordance rates • Incidence peaks from ages 20-40 • Incidence is similar in whites and Asians, but is somewhat decreased for African Americans
Graves' Disease • Autoimmune systemic disorder • Thyroid receptor antibody binding to and stimulating the TSH receptor • Excessive synthesis and secretion of thyroid hormone • Usually diffusely and symmetrically enlarged and firm
Hyperthyroidism—uptake • A. Normal • B. Graves’ Dz • C. Toxic Multinodular Goiter • D. Toxic Adenoma • E. Thyroiditis
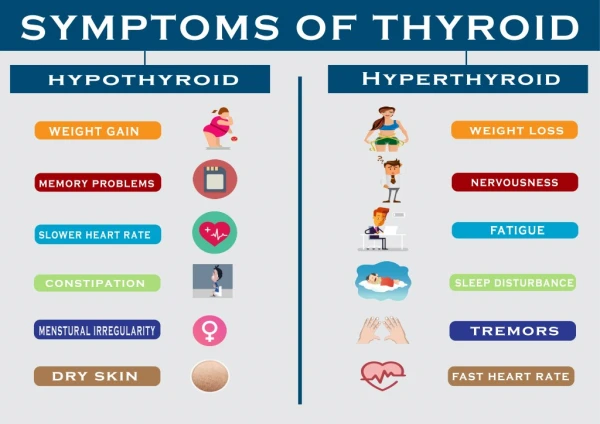
HyperthyroidismSymptoms • Heat intolerance, sweating, palpitations, fatigue • Weight loss, diaphoresis, increased stool frequency • Muscle weakness, anxiety, insomnia • Nervousness or restlessness; irritability, emotional lability • In women, irregular menses
HyperthyroidismClinical findings • Tremor, tachycardia (A. fib), • Goiter, lid lag, proptosis, periorbital edema, exophthalmos; chemosis; hyperreflexia • Warm, moist skin; dermopathy; and pretibial edema,osteoporosis
Lid Lag in Graves Disease Exopthalamos in Graves Disease
Hyperthyroidism—treatment • Beta-blockers: control sxs • Propranololdecr peripheral T4 -> T3 conversion • Graves’ Dz • PTU (safe in pregnancy) or methimazole • Rare side effect: agranulocytosis • Radioactive iodine • 75% of treated pts become hypothyroid • Surgery • Toxic Adenoma or TMNG • RAI or surgery
HyperthroidismSurgery • Surgical approach • Bilateral near-total or total thyroidectomy • Indication of surgery (In China) • Compressive symptoms • Secondary or adenoma • Recurrence of medicine or iodine-131 • No efficiency of medicine • Second trimester of pregnancy
Surgery for hyperthyroidismPreoperative preparation • Absolutely required • antithyroid drugs, for 3 to 6 weeks • with a goal of nearly normalizing the T3 and T4 • Propranolol or atenolol rapidly controls the adrenergic side effects of excess T4 and T3 • tachycardia, tremor, and diaphoresis • Lugol's solution rapidly but temporarily restores normal thyroid function and reduces thyroid gland vascularity
Surgical complications • Bleeding • Recurrent Laryngeal Nerve Damage • Hypoparathyroidism and Hypocalcemia • Superior laryngeal nerve damage • Thyroid storm
Thyroid cancerIntroduction • The most common, 95% of all endocrine cancers • Increasing faster than any other cancer • More than 90% , well differentiated • Good long-term prognosis
Thyroid cancerClinical Presentation • Most, clinically with a palpable nodule • Usually asymptomatic • Rare cases, with hoarseness, pain, dysphagia, dyspnea, coughing, or choking spells • Pain,with the suspicion for • Medullary thyroid carcinoma • Anaplastic carcinoma • Lymphoma
Pertinent historical factors predicting malignancy • A history of head and neck irradiation • Total body irradiation for bone marrow transplantation • Exposure to fallout from the explosion of the Chernobyl nuclear power plant in 1986, especially in children; • A family history of thyroid cancer; and rapid growth or hoarseness. • Children, men, and adults older than 60 years have an increased risk of malignancy
Increase the risk of thyroid cancer • Personal and family history of other endocrine disorders, • specifically hyperparathyroidism, pituitary adenomas, pancreatic islet cell tumors, adrenal tumors, and breast cancer. • A family history of papillary or medullary carcinoma (MEN syndromes), familial polyposis, Gardner's syndrome, and Cowden's syndrome
Pertinent physical findings Suggesting possible malignancy • Gritty texture”(颗粒样) of the thyroid nodule • Cervical lymphadenopathy • Vocal cord paralysis • Fixation of the nodule to surrounding tissue
Thyroid cancerDiagnosis • Ultrasound • Feature of malignancy • Irregular margins • Intranodular vascular pattern • Microcalcifications • Fine needle aspiration (FNA) • The most reliable and cost-efficient method
Thyroid cancer Diagnosis • Thyroid function tests • Serum markers • Thyroglobulin (TG) for well-differentiated thyroid cancer • Calcitonin and CEA for medullary thyroid cancer • All pts with medullary thyroid cancer • RET proto-oncogene • pheochromocytoma and hyperparathyroidism
Management of thyroid cancer The goals of therapy • Removal of primary tumor, disease that extends beyond the thyroid capsule, and involved cervical lymph nodes • Minimization of treatment- and disease-related morbidity • Accurate disease staging • Facilitation of postoperative treatment with radioiodine when appropriate • Accurate long-term surveillance • Minimization of the risk of recurrent local and metastatic tumor
Well-Differentiated Thyroid CarcinomaPapillary Thyroid Carcinoma • The most common endocrine malignancy,approximately 80% of new cases • Associated with the best prognosis • At least twice as common in women as men • A peak age of presentation of 38 to 45 years • 90% of radiation-induced,familial in 5%
Well-Differentiated Thyroid CarcinomaPrognoses • The risk of death • approximately 5% in the low-risk group • 40% in the high-risk group • Fortunately, most pts (70%) in the low-risk group
Other histological factors • To predict the behavior of thyroid cancer • Ploidy of the tumor • Adenylate cyclase response to thyroid stimulating hormone (TSH) • Radioiodine uptake • A positive positron emission tomography scan • Epidermal growth factor (EGF) receptor level and various gene profiles
Papillary Thyroid CarcinomaThe extent of surgical resection • Controversial • American recommondation • Total or near total thyroidectomycomplication rate of less than 2% • Selective nodal resection • Postoperative treatment with iodine-131 • Low-risk pts less than 1 cm • thyroid lobectomy and isthmectomy OK • Reoperation • multifocal, with nodal metastases, or with local invasion
Benefits of total thyroidectomy • Postoperative radioiodine scanning and ablative therapy can be effective • Serum thyroglobulin levels are rendered more sensitive for detecting recurrent or persistent disease • Intrathyroidal cancer that is present in more than 50% of patients is removed • The small risk of a differentiated thyroid cancer becoming an undifferentiated cancer is decreased.
Papillary Thyroid CarcinomaThe role of lymph node dissection • Also controversial • Micrometastasis to cervical lymph nodes is common (80%) • Prophylactic cervical lymph node dissection is not warranted • Functional neck dissection and central neck dissection should generally be performed • only in pts with clinical or sonographic evidence of lymph node involvement
Follicular Thyroid Carcinoma • Approximately 10% of all thyroid malignancies • Typically older than PTC • Usually in the sixth decade of life • The female-to-male ratio is between 2:1 and 5:1 • A slowly growing solitary thyroid nodule • A tendency to spread hematogenously • Rarely with symptoms of distant metastasis to the bone, lung, brain, and liver
Follicular Thyroid Carcinoma • Less than 6% metastasize to the cervical lymph nodes • Approximately 25% of pts have extrathyroidal invasion • 10% to 33% have distant metastasis at the time of initial diagnosis
The prognosis of follicular cancer • Slightly worse than that for papillary cancer • Overall survival ranges from 43% to 95% at 10 years • Lifelong surveillance is not necessary
The prognosis of follicular cancer • The important prognostic factors • Presence of metastatic disease • Older age (usually >40 years) • Degree of invasion (microcapsular vs. angioinvasion with or without capsular and widely invasive) • Degree of tumor differentiation
Follicular Thyroid Carcinoma • Diagnosis • The whole specimen must be evaluated for vascular and capsular invasion. • Diagnosis of follicular cancer cannot be made on FNAB
Follicular Thyroid Carcinoma • Treatment • The recommended initial operation is lobectomy and isthmectomy • Lymph node dissection is rarely warranted because nodal metastases are uncommon
Medullary Thyroid Carcinoma • 7% of thyroid cancers • 15% of all thyroid cancer–related deaths • Approx 75% sporadic零星的, 25% hereditary • From c cells or parafollicular cells • Located laterally at the junction of the upper two thirds of the thyroid gland at approximately the level of the cricoid cartilage
Medullary Thyroid Carcinoma • In the sporadic form • Usually a single focus of malignancy • Unilateral disease in 85% of cases • In the hereditary form • Multifocal and bilateral in 90% of cases • C-cell hyperplasia