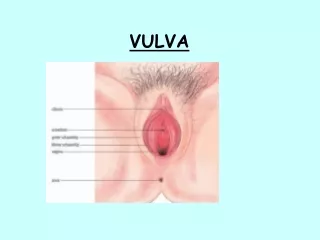
VULVA
480 likes | 752 Vues
VULVA. NORMAL HISTOLOGY Keratinizing stratified squamous epithelium (epidermis) Adnexal structures may be present- pilosebaceous units, and sweat glands May be involved by dermatoses that involve skin elsewhere.

VULVA
E N D
Presentation Transcript
NORMAL HISTOLOGYKeratinizing stratified squamous epithelium (epidermis) Adnexal structures may be present- pilosebaceous units, and sweat glands May be involved by dermatoses that involve skin elsewhere
NON-NEOPLASTIC ENTITIESBartholin's Cyst Common, all ages, secondary to obstruction, 3-5 cm Lined by transitional or squamous metaplasia Excised or opened permanently(marsupialization)
Vestibular Adenitis Chronic, Recurrent, Painful Unknown Etiology Treatment is surgical removal of inflamed mucosa
LICHEN SCLEROSISSlight increase in development of carcinoma(1-4%) however not considered a premalignant lesion
Pale, gray parchment-like skin with atrophy of labia and narrowed introitus most commonly seen in post menopausal women
Histologic features are epidermal atrophy with loss of rete pegs, homogenized collagen of papillary dermis and underlying band of lymphocytes.
SQUAMOUS HYPERPLASIAAcanthosis usually with hyperkeratosis and variable dermal inflammation Sometimes associated with carcinoma however it is not considered a premalignant lesion unless there is atypia
VULVA: BENIGH NEOPASMSSquamous PapillomaCondyloma Acuminatum- HPV(6 &11) induced squamous papilloma
Except in immunosuppressed individuals this may regress and is not considered a premalignant lesion Marker for sexually transmitted disease Papillary Hidradenoma- arises from apocrine sweat glands
Papillary Hidradenoma arises from apocrine sweat glands
PREMALIGNANT INTRAEPITHELIAL NEOPLASIADysplasia (vulvar intraepithelial neoplasia) ( VIN I-III )
HPV related in 90% of cases May be multicentric 5% of VIN III(severe dysplasia) progress to carcinoma elderly and immunosuppressed 30% associated with vaginal or cervical carcinoma
VULVAl CARCINOMA3% of all genital cancers in the female. 85% are squamous cell carcinoma 15%-basal cell carcinoma, adenocarcinoma 65% have metastasized to regional nodes(inguinal, pelvic) at time of diagnosis
Lesions less than 2 cm - 80% five-year survival rate Larger lesions with positive nodes have less than 10% five year survival rate
Verrucous carcinoma-well differentiated squamous cell carcinoma with features of condyloma. It has a good prognosis after wide local excision and is resistant to radiation.
Stage 0. During this stage, the cancer is a preinvasive disease called severe dysplasia, vulvar intraepithelial neoplasia (VIN), or carcinoma in situ (CIS).
This means that the lesion is still on the surface of the vulva and has not invaded more deeply. If detected early and treated, this stage cancer should be curable.
stages of invasive vulvar cancer.StageI. Cancer is only in the vulva or the space between the opening of the rectum and the vagina, (perineum), or both. The tumor is 2 cm or less in size. The lymph glands and other sites do not contain cancer.
Stage II. Cancer is in the vulva or the perineum, or both. The tumor is greater than 2 cm. The lymph nodes and other sites do not contain cancer.
Stage III. Cancer is found in the vulva or the perineum, or both. It has spread to nearby tissues such as the lower part of the urethra, the vagina, and the anus. It also may have spread to nearby groin lymph nodes. It has not spread to distant parts of the body.
Stage IV. Cancer has spread beyond the urethra, vagina, and anus into the lining of the bladder and the intestine. It may have also spread to lymph nodes on both sides of the pelvis, the groin, or to other parts of the body.
Recurrent. The cancer has come back after it has been treated. It may come back in the vulva or another place in the body.
VULVA: EXTRAMAMMARY PAGET'S DISEASELarge tumor cells lying singly or in small clusters within the epidermis and its appendages
The tumor cells contain mucopolysaccharides which stain positively with PAS, alcian blue and mucicarmine Underlying adenocarcinoma is uncommon
May be associated with carcinoma of breast, vulva or bladder-poor prognosis Otherwise it may persist for years without evidence of invasion The tumor can be present beyond the grossly apparent lesion resulting in recurrences
MALIGNANT MELANOMA5-10% of vulvar malignancies and 2% of all melanomas in women Peak incidence 6th to 7th decade Overall survival rate is 32% Histologically it may mimic paget's disease