Enhancing Medication Processes: Leveraging Technology for Patient Safety
500 likes | 627 Vues
This presentation by Jane Englebright, PhD, RN, Vice President of Quality at HCA, explores the critical need to re-engineer medication processes in healthcare to reduce errors and enhance patient safety. With a focus on technological advancements and evidence-based practices, the initiative aims for a 50% reduction in medication errors over the next 5 years. Key strategies include using electronic systems, barcoding, and standardized protocols to intercept potential errors and improve overall safety. The commitment to patient-centered care and continuous improvement is a cornerstone of this innovative approach.

Enhancing Medication Processes: Leveraging Technology for Patient Safety
E N D
Presentation Transcript
Re-Engineering Medication Processes to Capitalize on Technology Jane Englebright, PhD, RN Vice President, Quality HCA
% % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % U.K. % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % Switzerland % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % % Who is HCA? US 176 Hospitals 92 ASC’s in 22 States INTERNATIONAL 8 Hospitals
44,000 to 98,000 deaths/year 8th leading cause of death in US Provocative Statements: Most errors are caused by system failures rather than human error All manual processes are subject to error Many error reduction efforts do not take advantage of information systems Conclusions Status quo is not acceptable 50% reduction of error over next 5 years Institute of Medicine Reports on Medical Errors First Report: December 1999
HCA Patient Safety Goals • Establish patient safety as a visible commitment to putting patients first philosophy • Move from blaming people to improving processes • Improve use of technology to prevent and detect error • Use data to identify and measure improvements
HCA Patient Safety Initiatives Bring Evidence-Based Patient Safety Practices to HCA Facilities to Address Areas of Concern for HCA Each HCA Facility Implements Evidence-Based Patient Safety Practices in Areas of Concern for HCA Evidence-Based Patient Safety Practices: IOM Report ISMP Bates Areas of Concern for HCA: IOM Report Medication Safety Initiative
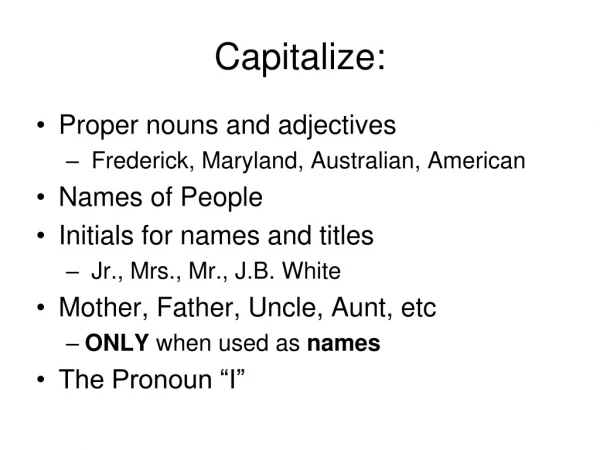
The Medication Safety Initiative Included: Rank Order of Error Reduction Strategies HCA Technologies Forcing Functions & Constraints Automation & Computerization Standardization & Protocols Checklists & Double-Checks Policies & Procedures Education & Information eMAR ePOM High Risk Med Protocols Practice Guidelines Competencies Awareness & Education
42% intercept 0 % intercept Errors resulting in ADEs 4% 6% Ordering Administration 34% Transcription 56% Dispensing Bates DW et al. Incidence of adverse drug events and potential adverse drug events. JAMA 1995;274:29-34.
Validates “Five Rights” of Medication Administration Requires patient specific clinical data for certain medications (i.e, pulse rate prior to administration Lanoxin, review of potassium level before giving Lasix). Sends a warning to alert nurse when the dose is to much or to little, or if the dose is being given to early or to late. Single “source of truth” for patient medication status. eMAR Safety Features
115,933,163 Doses administered in 171 hospitals 2,913,018 Error warnings 2,121,315 Doses not given after warning eMAR & Bar Coding:(Company-wide Results-Year 2005) Averted Errors
An interdisciplinary Steering Committee was responsible for planning; implementation; staff and physician education and management of any issues. eMAR Implementation Bar-coded Patient Armbands Electronic Safety Checking Bedside Verification Bar-coded Medication Doses Electronic Medication Administration Record & Charging
Fewer medication administration errors More complete documentation Staff perception of improved safety Patient perception of improved safety Improved accuracy of billing Expected Outcomes
Measurement Plan: Understanding the Impact Armband Audit
Physicians HCA Patient Safety Implementation Model Technology Change Hospital Process Change Culture Change
eMAR Works in Three Ways Policies, procedures, resource allocation systems Blunt End Process Redesign Direct caregiver Clinical Decision Support Sharp End ERROR Monitored Process Reports Results
Project Timeline6 – 7 months per hospital Post Implement Support Pre-Assessment Barcoding Meds, Hardware, Dictionary Changes, Testing End User Training Go Live Kick Off
Executive Walk-Arounds “Do No Harm” video “Verification” not “Scanning” Patient Safety Principles: Double-Check Implementation Activities: Culture
Functions Most Impacted . . . . Nursing Pharmacy Respiratory Care IT&S HIM Finance Quality & Risk Implementation Activities: Process
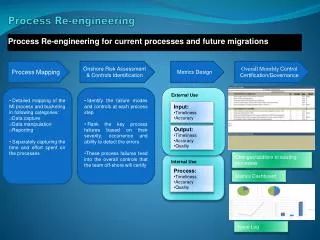
Process Re-Design • Develop a workflow study of the actual steps in the medication preparation and delivery process at your facility • Start at the patient and work backwards • Include Nursing, Respiratory Therapy, and Pharmacy
Model of care delivery Who do you want to give medications? Medication distribution system How do medications get from the pharmacy to the bedside? Nursing Impact
Accuracy and timeliness of order entry and turn around Bar Coding ALL medications Medication acquisition philosophy Override policy adherence Pharmacy Impact
“Wire Tie” Creativity
Workflow: Sequential vs Concurrent Therapy Scheduling of medication administration Medication storage and distribution Clear accountability for medication administration Non-standard medication preparations Order acknowledgement processes Respiratory Care Impact
New Member of the Clinical Team WLAN Installation and Support Computer Management Equipment Maintenance, including pharmacy equipment Downtime Processes IT&S Impact
Single MAR for each admission Incorporate into discharge printing process HIM Impact
Move to billing on Administration instead of billing as Dispensed Improved Audit accuracy Improved Charge capture Decreased paybacks from insurance audits Finance Impact
Explaining it all to the Surveyor Averted errors = Near misses Areas with 100% utilization rates can have zero medication administration errors Preserving Quality Control Activities Order Acknowledgement Chart Checks Quality & Risk Impact
Practice Recommendations
Carts should be cleaned at least daily with hospital approved disinfectant Carts may be used in isolation rooms Carts should be cleaned before leaving the room if contaminated and when used in isolation Patient Safety equipment can be safely used in all patient care areas – exception: Known SARS or Small Pox Infection Control Recommendations
Identify armband solution Newborn Pre-registration Processes Unit dose medications Bar code identification of Breast Milk and documentation of feeding Pediatric/NICU Recommendations
Don’t take the scanner into seclusion Consider alternative form factors for scanners Unit dose medications Special armband needs Psychiatric Recommendations
Implementing eMAR • Roll out in waves • Bring up first 1 or 2 units • First unit that mostly discharges patients • Maintain for 1-2 weeks • Troubleshoot and resolve issues as they arise • Roll out remaining units quickly in related waves • Turn on Admin Billing
Packaging and labeling errors in pharmacy Changing federal regulations Emerging barcode symbologies Invalidating bedside verification with workarounds Project Risks
eMAR & Bar Coding Accountability Structure HCA Corporate Quality HCA IT&S Organization Advisory Groups Operational Accountability Structure
Getting Staff to Use the Technology • “How is this going to help me do my job better?” • “Why is this necessary?” • “I didn’t go to school to become a computer genius!” • “I guess this keeps somebody employed!” • “Just when I thought I had myself organized, they come up with something new!”
Answering the “Why?” • Keep the team engaged. Be patient as many do not adapt to change readily • Communication…e-MAR benefits vs. expectations • Focus on patient knowledge and patient safety • Ongoing involvement of core team • Keep the team focused on Patient Safety as a priority goal
“Get it Right” • Equipment Analysis • Pilot FIRST!!!! • Communication • Training/Education • Troubleshooting Plan • Competency • Ongoing unit based resources
Staff Meetings PATIENT SAFETY STRESSED Expectations clearly communicated again Non-compliance outcomes discussed Accountability Mandatory Education & Competency Assessment Regular monitoring of usage reports Prompt follow-up on negative usage patterns Leadership Strategies
Leadership Makes a Difference Results from pilot hospital: • Usage STATS improved within one week of implementing accountability plan. • No formal disciplinary measures were required. • Satisfaction scores improved!!! Goal 90 – 100%
Results • Averted Errors • Usage • Staff Perception
First & Second quarter summary reports Malpractice claims related to medication administration have decreased by 16%
Pharmacy Perception Survey I believe use of the eMAR and bar coding system is reducing medication errors in my hospital.
Pt. history - allergies etc… Lab link Reminder to document BP/HR/Pain Scale Checks and balances Look alike sound alike drugs… Unusual doses flagged Realistic expectations Novice Staff Rely on e-MAR!
eMAR Maintenance Work • Software • Equipment • Culture transformation • Process change
The Way We Do Meds at HCA Single point of accountability within each hospital to assure optimal ongoing operation Corporate eMAR Advisory Committee to address Culture-Process-Technology issues Regular division meetings Monthly conference calls/Quarterly web casts for sharing best practices and enhancements eMAR & Bar Coding