Absorption
270 likes | 716 Vues
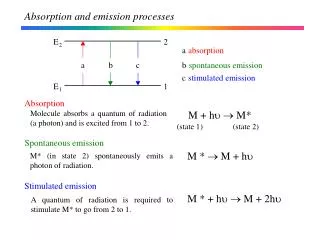
Absorption. Affected by physiological factors route of administration drug distribution drug chemical physical properties dissolution rate (solids) hydrophilicity/hydrophobicity. Pathways of Oral Absorption. Two main mechanisms of transport across the gastrointestinal membrane:

Absorption
E N D
Presentation Transcript
Absorption • Affected by • physiological factors • route of administration • drug distribution • drug chemical physical properties • dissolution rate (solids) • hydrophilicity/hydrophobicity CHEE 440
Pathways of Oral Absorption Two main mechanisms of transport across the gastrointestinal membrane: Transcellular diffusion Paracellular diffusion CHEE 440
Transcellular Diffusion The transcellular pathway is composed of 3 mechanisms: passive diffusion, carrier-mediated transport, endocytosis Passive diffusion CHEE 440
Partition coefficient, Ko/w • for absorption into cell, drug must pass through lipid cell membrane • consider two immiscible phases (oil and water) and a drug which is soluble in both (ex. cyclosporine), at equilibrium. oil water ideal and ideally dilute solutions : CHEE 440
Clinical Significance of Ko/w • prediction of absorption of drugs through various tissues • absorption of acidic drugs from colon • absorption of basic drugs from small intestine CHEE 440
Partition Coefficient and Absorption Optimum Ko/w CHEE 440
Carrier-Mediated Transport • Active transport CHEE 440
Drug Solubility • Solubility: the extent to which a drug dissolves under a given set of conditions of solvent and temperature • significance • drugs must be in solution before they can be absorbed • drugs of low aqueous solubility present formulation problems • saturation concentration, Csat • limit of solubility of a solute in a solvent at a given T CHEE 440
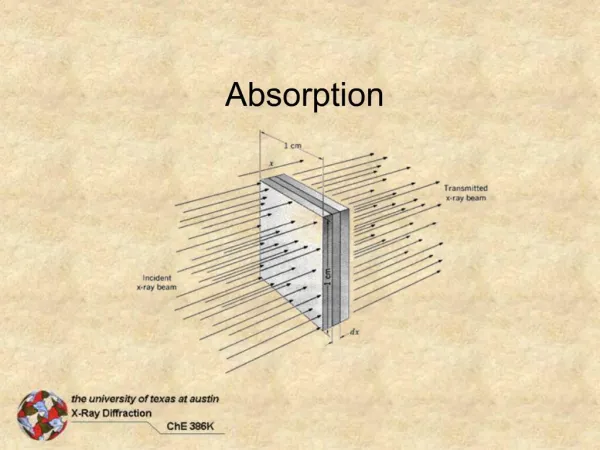
Csat C = Cb Dissolution Rate • important for tablets, capsules, suspensions • slow dissolution rate = low bioavailability • consider a solid particle in water stagnant water layer Noyes-Whitney Eqn CHEE 440
Dissolution Rate • But, surface area changes with time; • for spherical particles: • for N particles: r = radius at time t ro= initial radius r = density M = mass of particles k = cube-root dissolution constant CHEE 440
Factors influencing Csat • crystal structure: polymorphism, hydrates • pH • salt form • common ion effect • co-solvents CHEE 440
crystal solid + solvent + dissolved solute Process of Dissolution CHEE 440
Crystalline Solids • regular, ordered structure • composed of identical repeating units - unit cell • ex. cubic, rhombic, tetragonal • have distinct melting pts • strength of bonds between atoms, molecules determines : • geometry of unit cell • Tf, CHEE 440
Crystalline Solids • Electrostatic, Covalent Bonds • ex. NaCl, graphite (C4) • strong bonds - cubic unit cell • hi Tf, hi (eg. Tf= 801°C for NaCl) • stable structure • hard, brittle CHEE 440
Crystalline Solids • Van der Waals, H-bonds • ex. organic compounds • weak bonds • low Tf, low (e.g. Tf = 238°C for caffeine) • soft materials • metastable structures CHEE 440
Polymorphism • molecule can crystallize into more than one crystal structure • metastable form transforms to stable form over time • usually nonreversible process - monotropic polymorphism • many polymorphic forms possible • progesterone - 2 • nicotinamide - 4 • dissolution rate changes with polymorphic form CHEE 440
Amorphism • no crystal structure • no distinct Tf • supercooled liquids - subdued molecular motion • flow under an applied pressure • generally easier to dissolve CHEE 440
Crystal Hydrates • solvent trapped when compound crystallizes - solvates • solvent is water - hydrates • no water - anhydrate • solvent-compound interactions • H2O further stabilizes lattice - polymorphic solvates • H2O occupies void spaces - pseudopolymorphic solvates CHEE 440
Crystal Hydrates • anhydrate has higher Tf, generally dissolves faster CHEE 440
Crystal Hydrates • Significance • incorporation of H2O affects bioabsorption rate and bioactivity CHEE 440
pH and solubility • weakly acidic drug • pHp the pH below which the drug precipitates from solution • weakly basic drug • pHp the pH above which the drug precipitates from solution CHEE 440
Drug Salt Form • salt solubility depends on nature of counter-ion CHEE 440
Slightly Soluble Electrolytes • ex. Al(OH)3, Ca2CO3, ZnO, drug salts AgCl(s) Ag+(L) + Cl-(L) Ksp = [Ag+] [Cl-] = 1.25(10-10) at 25°C Al(OH)3 Al3+(L) + 3OH-(L) Ksp = [Al3+] [OH-]3 = 7.7(10-13) at 25°C • beware of common ion effect (salting-out) CHEE 440
Other solubility issues • cosolvents • solvents which, when combined, increase the solubility of a given compound • ex. phenobarbital in water has a solubility of 0.1g/100 ml, in alcohol 1 g in 10 ml, and in 20% alcohol/water 0.3 g/100 ml • combined effect of pH and cosolvent • adding alcohol to buffered solution of weak electrolyte increases solubility of undissociated form • decreases pHp for a weakly acidic drug CHEE 440
pH and Ko/w • dissociated portion of drug does not dissolve in oil phase • partition coefficient • apparent partition coefficient CHEE 440
pH and Ko/w • as change pH, add common ion, [HA]w changes weak acid : weak base : CHEE 440
Summary • Absorption of drug is influenced by combination of permeability and solubility • Implications of Low Drug Permeability • incomplete absorption • rapid, complete dissolution needed • release may need to be modified • increase exposure to an absorption window • possible retarded release if a saturable transport phenomenon exists • Implications of Low Drug Solubility • will have to optimize particle size • consider salt forms, polymorphs, hydrates, co-solvents CHEE 440