Hemostasis and Blood Coagulation
190 likes | 838 Vues
Hemostasis and Blood Coagulation. BS 4 th Semester Arsalan Yousuf. Hemostasis. Prevention of blood loss. Achieved through following mechanisms: Vascular constriction, (2) Formation of a platelet plug, (3) Formation of a blood clot as a result of blood coagulation,

Hemostasis and Blood Coagulation
E N D
Presentation Transcript
Hemostasis and Blood Coagulation BS 4th Semester Arsalan Yousuf
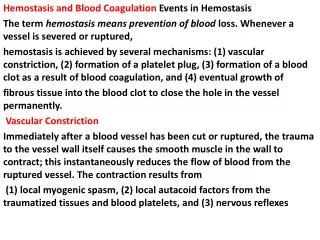
Hemostasis • Prevention of blood loss. Achieved through following mechanisms: • Vascular constriction, • (2) Formation of a platelet plug, • (3) Formation of a blood clot as a result of blood coagulation, • (4) Eventual growth of fibrous tissue into the blood clot.
Vascular Constriction • After a blood vessel has been cut or ruptured, the trauma to the vessel wall causes the smooth muscle in the wall to contract. • Local myogenic spasm, • (2) Local autacoid factors from the traumatized tissues and blood platelets, • (3) Nervous reflexes. More vasoconstriction results from local myogenic contraction of the blood vessels initiated by direct damage to the vascular wall. The platelets are responsible for much of the vasoconstriction by releasing a vasoconstrictor substance, Thromboxane A2 Formation of the Platelet Plug If the cut in the blood vessel is very small the cut is sealed by a platelet plug, rather than by a blood clot.
Platelets • Platelets (thrombocytes) are minute discs 1 to 4 μm in diameter. • Formed in the bone marrow from megakaryocytes, • The normal concentration of platelets in the blood is between 150,000 and 300,000 per μL. COMPONENTS Actin and myosin molecules. Residuals of both the Endoplasmic Reticulum and Golgi apparatus. Mitochondria and enzymes that are capable of forming ATP. Fibrin-stabilizing factor. A coat of glycoproteins that repulses adherence to normal endothelium. Half life of 8 to 12 days.
Platelet Plug When platelets come in contact with a damaged vascular surface, they immediately change their own characteristics. • Begin to swell; • Assume irregular forms with numerous irradiating pseudopods; • Release granules that contain multiple active factors; • Become sticky and adhere to collagen in the tissues and to a protein called von Willebrand factor that leaks into the traumatized tissue from the plasma; • Secrete large quantities of ADP; • Enzymes form thromboxane A2. • ADP and thromboxane in turn act on nearby platelets to activate them as well.
Blood Coagulation in the Ruptured Vessel Blood clot begins to develop in 15 to 20 seconds if the trauma to the vascular wall is severe, In 1 to 2 minutes if the trauma is minor. • Once a blood clot has formed, it can follow one of two courses: • It can become invaded by fibroblasts, • It can dissolve
Mechanism of Blood Coagulation The Basic Theory Whether blood will coagulate depends on the balance between Coagulants and Anticoagulants.
Thrombin and Fibrinogen • Prothrombin is a plasma protein, an alpha2-globulin, having a molecular weight of 68,700. It is present in normal plasma in a concentration of about 15 mg/dl. • Unstable protein • Produced continuously in the liver. Vitamin K is important for its formation. • Thrombin in turn acts as a serine protease that converts soluble fibrinogen into insoluble strands of fibrin, as well as catalyzing many other coagulation-related reactions.
Vicious Circle of Clot Formation A clot itself initiates a vicious circle (positive feedback) to promote more clotting. Thrombin has a direct proteolytic effect on prothrombin itself, tending to convert this into still more thrombin. Initiation of Coagulation Formation of Prothrombin Activator Extrinsic Pathway Intrinsic Pathway
Extrinsic Pathway for Blood Clotting Begins with trauma to the vascular wall and surrounding tissues
Intrinsic Pathway for Blood Clotting Begins in the blood itself. Factor VIII is the factor that is missing in a person who has classic hemophilia, for which reason it is called antihemophilic factor. Platelets are the clotting factor that is lacking in the bleeding disease called thrombocytopenia.
Importance of Calcium ions • Except for the first two steps in the intrinsic pathway, calcium ions are required for promotion or acceleration of all the blood-clotting reactions. • When blood is removed from a person, it can be prevented from clotting by reducing the calcium ion concentration. • The extrinsic pathway can be explosive. The intrinsic pathway is much slower to proceed, usually requiring 1 to 6 minutes to cause clotting.