ACUTE AND CHRONIC INTERSTITIAL NEPHRITIS
600 likes | 1.18k Vues
ACUTE AND CHRONIC INTERSTITIAL NEPHRITIS. PROF. Dr . MARLEEN PRAET, MD, PHD University Hospital Ghent Belgium. Interferences with the interstitium: broad spectrum. Infection : direct (BK virus, TBC, acute pyelonephritis), indirect( βStreptococci) Immunologic Allergic: drug – induced

ACUTE AND CHRONIC INTERSTITIAL NEPHRITIS
E N D
Presentation Transcript
ACUTE AND CHRONIC INTERSTITIAL NEPHRITIS PROF. Dr . MARLEEN PRAET, MD, PHD University Hospital Ghent Belgium
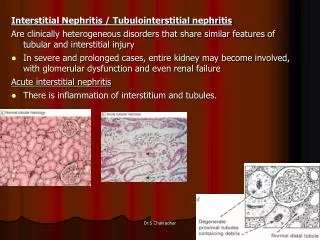
Interferences with the interstitium: broad spectrum • Infection: • direct (BK virus, TBC, acute pyelonephritis), • indirect( βStreptococci) • Immunologic • Allergic: drug – induced • Auto-immune: Sjögren syndrome • Alloimmune: acute cellular allograft rejection • Unknown: IgG4- associated acute interstitial nephritis • Toxic: Pb poisoning, cadmium poisoning, Balkan endemic nephropathy • Metabolic: oxalosis secondary to malabsorbtion , gout • Obstruction: ureteral- pelvic junction stenosis: • Radiation: radiation interstitial nephritis • Idiopathic: sarcoidosis
What is the program: • Morphology of the interstitium • Importance • Different entities of interstitial disease • Appearances are often similar despite varied mechanisms • Search for etiologic agent, distinctive features: granuloma, eosinophils, crystals, viral inclusions
Morphology of the interstitium • Composed of a loosely organized matrix consisting of the collagen types I and III, proteoglycans containing the “interstitial cells”: • matrix producing fibroblasts • macrophages • dendritic reticulum cells • endothelial cells
Morphology of the interstitium • Fibrosis develops after infiltration by mononuclear cells (lymphocytes) which is accompanied by deposition of fibronectin, collagen type I, III, VI and IV. • There is a physiological balance between ongoing matrix formation and - degradation.
Importance of interstitial cells • Interstitial fibroblasts: • Fibrogenesis • Production of erythropoietine (they lose this function during the process of fibrogenesis) • Can transform into myofibroblasts (expression of SMA) • Changes in the interstitial area play an important negative predictive value on the long term follow up of the primary kidney disease. Important and determining factors are interstitial volume (=fibrosis) and inflammation
Different entities of interstitial disease • Acute interstitial nephritis • Chronic interstitial nephritis • Acute pyelonephritis • Chronic pyelonephritis (reflux related) • Xanthogranulomatous pyelonephritis • Malakoplakie • Myeloma kidney • IgG4 interstitial nephritis • Lead induced interstitial nephritis • Urate nephropathy • TX related Polyoma induced interstitial nephritis • Balkan interstitial nephritis
Acute interstitial nephritis • Most common etiologies are: • a) those related to the use of medications: 85% • b) those related to infectious agents: 10% • c) those associated to systemic disease or glomerular diseases: 1% • d) idiopathic disease: 4%
Acute interstitial nephritis: drugs • Etiology: AB (penicillins and cephalosporins, methicillin), diuretics, NSAID’s, chinese herbs, lithium • Pathogenesis: T cell mediated allergic - immune reaction on drug or drug-self protein conjugate (hapten) later followed by accumulation of lymphocytes, plasmocytes and histiocytes • Histology: • Early signs: oedema, lymphocytes focally • Later: eosinophils, lymphocytes, plasmocytes and histiocytes with granuloma formation(with giant cells) in 30 %, especially after AB • Tubulitis (distal tubules): with breaks of TBM, necrosis of tubular cells and atrophy and loss of tubules. • Tamm Horsfall may find its way to the interstitium (DD obstruction of nephron).
Acute drug induced interstitial nephritis Oedema and focal inflammation Granuloma EOS
Acute drug induced interstitial nephritis • Normally are the glomeruli not afflicted. • One exception: use of NSAID’s: can combine ARF with Nephrotic Syndrome (effect of cell- mediated lymphokine directed reaction) inducing Minimal Lesions (effacement of foot processes of podocytes)
Acute interstitial nephritis: clinics Acute Renal Failure and reduced glomerular filtration rate: • depends on the severity of inflammation • interstitial oedema causes elevated intratubular pressure • intratubular obstruction through intra luminal cells • tubular backleak • vasoconstriction • tubuloglomerular feedback
Recovery? Drug withdrawal: 60-90% in 1 to 12 mths Irreversible with analgesics, NSAIDs, longterm use Adverse prognostic features Marked interstitial inflammation Granuloma (50% irreversible) Tubular atrophy Fibrosis Outcome of drug- induced interstitial nephritis
Acute interstitial infectious nephritis • Infectious:direct invasion or remote infections bacteria (ß hemolytic streptococci), parasites (Leishmania) and viruses (EBV, measles) • Pathogenesis: immunological hypersensitivity reaction to the infectious agent, effect of chemokines produced by the kidney in response • Histology: • Early signs: invasion by lymphocytes, eosinophils around the veins • In casu there is tubular destruction: histiocytes accumulate • Tubulitis with disappearance of the brush border in proximal tubules
Acute interstitial nephritis: systemic • Association with: Goodpasture syndrome, lupus nephritis, mixed cryoglobulinemia, membranoproliferative glomerulonephritis
Chronic interstitial nephritis • Etiology: chronic drug intake (analgesics, lithium), urinary obstruction, chronic reflux, • Pathogenesis: persistence of damageing factor: ischemia, chronic immune reaction • Histology: fibrosis + diffuse infiltration by lympho’s, plasmo’s, histiocytes (with granuloma). Tubular changes (atrophy, compensatory hypertrophy with microcystic changes) • Beware of: • Papillary necrosis, - sclerosis and- calcification: due to sclerosis of the capillaries under the urothelial epithelium • Tumor development: papillary tumors, multifocal
Interstitium in transplants • Calcineurin inhibitors: • Heart, liver, pancreas, kidney transplants in different doses • Different levels of interstitial damage • Most structural nephrotoxic effects in arterioles and glomeruli are manifestations of Thrombotic MicroAngiopathy(TMA) with different patterns of severity. The interstitial fibrosis has an uncertain pathogenesis but is probably vascular.
Cellular rejection in kidney Tx • Histology: • Very early: eosinophils • Followed by T lymphocytes • Later: Plasmocytes IgG+ if IgM+ : be aware of polyoma infection • In peritubular capillaries (PTC): lymphocytes++
Cellular rejection Tubulitis CD3
Acute pyelonephritis • Etiology: ascending infection from the pyelon • Pathogenesis: microbial release of degradative enzymes and toxic molecules, direct contact or penetration of the host cell by the infectious agent and the inflammatory response mediated by antibodies, T cells • Histology: • Tubules are damaged by neutrophils (Congored)
Chronic pyelonephritis • Etiology: reflux • Histology: - wedge shaped interstitial fibrosis(follows the traject of the papillae and ascending tubules) accompanied by tubular atrophy, vascular atheromatosis, glomerular sclerosis, inflammation - outside the wedges: normal parenchyma but with secondary changes in the glomeruli: glomerular hypertrophy, FSGS
Xanthogranulomatous pyelonephritis • Etiology: chronic ascending infection: lithiasis, pyelal or ureteral tumors, ureter stenosis. The infective organisms are E. Coli, Proteus sp, Klebsiella, Pseudomonas, Enterococcus • Histology: • accumulation of histiocytes in the interstitum containing PAS/Diastase resistant granules in the cytoplasm • fibrosis • chronic inflammatory cells
Malakoplakia • Etiology: accumulation of phagolysosomes in the cytoplasm of macrophages containing bacteria in various stages of breakdown. • Histology: identical to xanthogranulomatous pyelonephritis but with presence of Michaelis Gutman bodies: these are PAS +, von Kossa positive (calcium+), Perls + round lamellar structures measuring 4 tot 10 µ
Granulomatous interstitial nephritis • Sarcoidosis: naked granulomas in cortex with Langhans giant cells: 29 % • Drug induced interstitial nephritis (AB):45% • Infection: TBC, fungal infections • Gout: urate granuloma • Cholesterol granuloma
Myeloma kidney or CAST nephropathy • Differentiate from other light chain entities: excretion of light chains due to plasma cell dysfunctions (MGUS, myeloma, Waldenström lymphoma) can be accompanied by deposits of light chain in the kidney: where? • Glomeruli: LCDD • Tubules: Cast nephropathy or myeloma kidney • TBM: atypical LCDD with deposition of monotypic kappa light chain deposits • Interstitium: secondary inflammation • Vessels: LCDD
How to differentiate? • Good lightmicroscopy • Immunohistochemistry/Immunofluorescence • Electronmicroscopy
Distinctive patterns LM- IF IF- EM
TUBULES Intraluminal casts: LM: hard casts, birefringent, dual colored, giant cells IF: Kappa 60%, Lambda 40% EM INTERSTITIUM Inflammation CASTNEPHROPATHY
Polyoma Nephropathy • Reactivation of a latent endogenous virus in immune incompetent patients • Nephropathy usually presents during the first year after transplantation
Polyoma Nephropathy • Histology: • Viral replication produces nuclear inclusions and cell necrosis (urothelium, tubular epithelium) • T and B lymphocytes, plasmocytes, histiocytes accompany the necrosis with plasma cell tubulitis • Starts in the medulla • Progression is marked by tubular atrophy, interstitial fibrosis and graft loss
Balkan endemic nephropathy • Where?: Croatia, Bosnia, Serbia, Bulgaria, Romania with prevalence between 2% and 10% • Pathogenesis: unknown: genetic predisposition, role played by coronavirus, heavy metals, ochratoxin, mycotoxins
Chinese Herbs Nephropathy • 1992 and 1993: slimming regimen containing Chinese Herbs: Stephania tetrandra. • Role played by aristolochic acid forming premutagenic adducts with DNA in the kidney and urothelium:patients developed renal failure and TCC 5 months later
Chinese Herbs Nephropathy Cosyns JP. Drug Safety 2003, 26 : 33-48 Stephania