Obstructive jaundice
1.14k likes | 1.74k Vues
بسم الله الرحمن الرحيم. Obstructive jaundice. Presented by: DR .Mohammed Yousif Al Alim. Contents. Definition. Metabolism of bilirubin. Anatomy of the biliary system. Causes of obstructive jaundice. Clinical presentation. Diagnosis. Management. Complications.

Obstructive jaundice
E N D
Presentation Transcript
بسم الله الرحمن الرحيم Obstructive jaundice Presented by: DR .Mohammed Yousif Al Alim
Contents • Definition • Metabolism of bilirubin • Anatomy of the biliary system • Causes of obstructive jaundice • Clinical presentation • Diagnosis • Management • Complications • Post operative jaundice
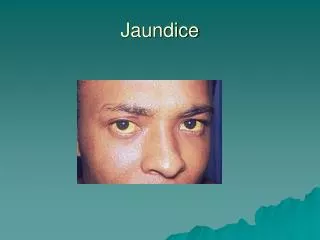
Introduction Jaundice or icterus yellowish discolouration skin, mucous membranes, Due to. excess plasma bilirubin Normal range Is <1mg/dl Clinically obvious When it is>3mg/dl 1mg/dl=17mmol/l
Definition OF OBSTRUCTIVE JAUNDICE: A condition where blockage of bile flow causes over spills of bile products into the blood &incomplete bile excretion from the body
Metabolism of bilirubin Produced in the reticuloendothelial sysetm break down of haem Carried to the liver bound to albumin Within the hepatocytes it is cojugated by Glucouronyl transferase into bilirubin glucouronide Which secreted by the bile canaliculi In the intestine it is reduced by the bacterial flora into urobilinogen ,small amount is excreated in the stool stecobilinogen The remainder reach the liver to enter the enterohepatic circulation
Surgical anatomy of the biliary system Composed of Rt & Lt hebatic duct which unite at the porta hepatis To form the common hepatic duct Which join cystic duct to form the common bile duct The CBD is 11-12cm in length & 4-10 mm in diameter it is devided into supraduodenal,retrodudenal,interapancreatic & interaduodenal part it then joined the pancreatic duct to opened in the 2nd part of the duodenum in the major duodenal papilla Gall bladder is pear-shped sac 10cm in length Commposed of fundus body & neck Blood supply by the cystic artery
Aetiology of obstructive jaundice Common Common bile duct stones Carcinoma of the head of pancreas Lymph nodes in the porta hepatis Infrequent carcinoma Ampullary Pancreatitis Liver secondaries Rare Benign strictures - iatrogenic, trauma syndromeMirriz’s cholangitissclerosing Cholangiocarcinoma atresia Biliary cystschoydochal
Anatomical classifications • Obstruction within the lumen: • stone or parasite • Pathology within the wall • *atresia of CBD • *tumor of the bile duct • *traumatic stricture • *chronic cholangitis • External compression; • *tumor of the head of pancreas • *periampullary tumor • *chronic pancreatitis
Clinical features • Yellowish discoloration of the skin & mucous membrane • Dark urine • Pale stool • pruritis
physical examination • Deep jaundice • High fever and chills suggest a coexisting cholangitis • Imatiated • Scratch marks on the skin • Pruses on the skin suggestive of vitK defeciency • Bradycardia • Gallbladder may be palpable (Courvoisier sign).. • There may be ascites associated associated with cirrhosis.. • . Malignancy is associated with the absence of pain and tenderness during the examination. • .
Investigation of obstructive jaundice Aims: • TO confirm the diagnosis • To know the type of jaundice • To detect the underline cause • To detect the complications • TO ASSES THE FITNESS FOR SURGERY
Urinalysis • Macroscopic appearance of the urine • Presence of bile pigment • Absence of urobilinogene strips are very sensitive to bilirubin, detecting as little as 0.05 mg/dL. Thus, urine bilirubin may be found even in the absence of hyperbilirubinemia or clinical jaundice
Serum bilirubin • Doesn’t give aclue about the the cause of obstruction • Conjugated & unconjugatd • Extra hepatic obstruction; • inetially it is mainly cnjugated,but later on the • uncojugated is rises • Intera hepatic obstruction; • both conjugated & unconjugated are rise
Liver enzymes ALP secreatd from the endothelum of the biliary canaliculy,not specific,unless it is associated with elevation in GGT The degree of elevation may be used in the differentiation between extera & interahepatic obstrution AST mild to moderate in extera hepatic obstruction ALT both of them are elevated in interahepatic obsruction *A 3-fold or more increase in ALT strongly suggests pancreatitis
Prothrombin time (PT): • This may be prolonged because of malabsorption of vitamin K. • Correction of the PT by parenteral administration of vitamin K may help distinguish hepatocellular failure from cholestasis. .
Renal function test • Blood urea • Serum creatinine • Serum electorolytes
Imaging study Plain X- Ray of the abdomen 10% Gallstones Radio-opague *It domensterate: • Gas in GB or biliary tree • Calcification of GB
U/S abdomen Accuracy>90% • Shows; • *stones in the GB & biliary tree • *Size of GB & thickness of it’s wall • *Dalitation in the biliary tree • *Diameter of the CBD • *Pancrease inflammation or tumor • *Liver parynchyma & texture *Differntiate intera hepatic from extera hepatic causes The presenc of normal CBD Diameter doesn’t exclude obstruction =recent & intermittent obstruction
Advantage:cheap available noninvasive Disadvantage :doesn’t detect *small stones *,stones in the distal part of CBD *doesn’t give aclue about site & extent of lesion. *Un satisfactory in obese,ascites,previous surgery gaseous distention u/s Abdomen
CT abdomen • detect spcific cause & level of obstruction • More accurate • can be used with contrast to see biliary tract,pancreatitis &tumour Disadvantage:less accurate in small CBD stones ,expensive,hazard of radiation Used if US is found to be technically difficuilt
MRI • Excellent soft tissue detection • Can be used in any plane • No hazard of radiation
Magnetic resonance cholangiopancreatography MRCP • Detect stones as small as 2 cm • High specificity & sensetivty rate • Detect CBD tumor staging • Pancreatic lesion :tumours ,ca ampulla T2:ability of molecule to move from place to another T1:ability of the molecule to return to that place Fluids(bile & pancreatic) have rabid T2 phase MRCP has ability to detect molecule with rabid T2 phase
Endoscopic retrograde cholangiopancreatography: ERCP • ERCPis procedure that combines endoscopic and radiologic modalities • To visualize both the biliary and pancreatic duct systems. • Endoscopically, the ampulla of Vater is identified and cannulated. • A contrast agent is injected into these ducts • And x-ray images are taken to evaluate their caliber • length, and course • .
ERCP • *Accuracy>90% • useful for lesions distal to the bifurcation of the hepatic ducts • Ductal stones,tumour of CBD &PANCREASE sclerosing cholangitis • Has diagnostic & therapiotic modalities • Sphincterotomy,exteraction stones,insertion of stent • *Disadvantage: • limited capacity to image the biliary tree proximal to the site of obstruction • In ability to visualize intera hepatic biliary system • *Complications: haemorrhage ,acute pancreatitis,cholangitis,duodenal perforaion, • impacted dormia basket,gall stone illeus,
ERCP • DIFFICULTIES: • Duodenal or pyloric stenosis • Bypass operation:cholecystojuojenostomy • Uncooperative pt • Inexpert personnel Mortality 0.1%when used diagnostic 10% when used therapeutic
MRCP versus ERCP MRCPhas the same diagnostic accuracy to ERCP except for acute pancreatitis MRCP is noninvasive MRCP can be used in distorted anatomy MRCP can visualise interahepatic biliary tree MRCP can only be used as diagnostic modalities
Radionuclide scanning • technetium iminodiacetic acid • Taken up by hepatocytes and actively excreted into bile • Allows imaging of biliary tree • Failure to fill gallbladder = acute cholecystitis • Delay of flow into duodenum = biliary obstruction
Percutaneous transhepatic cholangiogramPTC • Sedative should be used • The liver is punctured by CHIBA 22 needle to enter the intrahepatic bile duct system. • An iodine-based contrast medium is injected into the biliary system and flows through the ducts. • Obstruction can be identified on fluoroscopic monitor • Pt should be covered by antibiotics. • VitK or fresh plasma should be given • Indication: failure ofERCP or in ability to detect proximal lesion
PTC • Complications • allergic reaction to the contrast medium, • peritonitis with possible intraperitoneal hemorrhage, sepsis, cholangitis, subphrenic abscess • lung collapse. • *Severe complications occur in approximately 3% of cases