CARDIOTONICS AND CORONARY VASODILATORS
960 likes | 1.36k Vues
CARDIOTONICS AND CORONARY VASODILATORS. NURS 1950: Pharmacology I. Objective 1: describe the relationship of calcium to electrical activity of the heart Resting: Preload: Afterload :. repolarization. Heart dependent upon influx of calcium

CARDIOTONICS AND CORONARY VASODILATORS
E N D
Presentation Transcript
CARDIOTONICS AND CORONARY VASODILATORS NURS 1950: Pharmacology I
Objective 1: describe the relationship of calcium to electrical activity of the heart • Resting: • Preload: • Afterload:
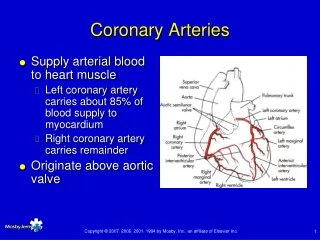
repolarization • Heart dependent upon influx of calcium • Ca+ enters channels in the cardiac cell membrane and go into the cell along with Na • K+ comes out • Cardiac cells contract
The ANS is the primary controller of heart rate • Cholinergic (parasympathetic) vagal fibers are close to the SA node • Stimulation with acetylcholine slows the heart rate
Sympathetic (adrenergic) nerves also innervate the heart • Stimulation causes norepinephrine to be released. • Increases heart rate, slows refractory period
Objective 3: describe how cardiac drugs affect cardiac action
How cardiac drugs work • 1. Increase or decrease the force of myocardial action • Positive inotropics • Negative inotropics
2. Increase or decrease heart rate by altering SA node impulse conduction • Positive chronotropics • Negative chronotropics
3. Increase or decrease conduction of AV impulses • Positive dromotropics • Negative dromotropics
Cardiac glycosides • Digoxin & relatives • Come from Natural sources • Helpful in CHF • Have a positive inotropic effect
Increases mechanical efficiency of heart • This pumps more blood • With increased blood to kidneys, diuresis occurs, edema reduced • Cardiac glycosides also have negative chronotropic effect, • Negative dromotropic effect
Action • Thought that they cause release of free calcium within the cardiac muscle cell • Also change the electrical activity of myocardium
Decrease velocity of electrical conduction, prolong refractory period in AV conduction system • Increase vagal tone
Objective 5: relate how the effects of digitalis are beneficial to the client with CHF • Recall the signs/symptoms of CHF • How do you think cardiac glycosides improve this condition?
Objective 6: describe the usefulness of digitalis in the treatment of atrial fibrillation
What is atrial fibrillation? • What activity of the cardiac glycosides improve this condition?
Chronotropic/dromotropic effects • Suppress impulse conduction through the AV node • This prevents excessive atrial activity from reaching ventricles
Objective 7: list the generic and brand names of the digitalis preparations • Digitalis preparations similar in pharmacological properties, toxic effects
Prototype • Digoxin (Lanoxin, Lanoxicaps): oral or IV • Onset 30-120 minutes oral • Peaks 2-6 hrs • Duration 2-4 days • Eliminated by kidney • Used most often as rapid onset, short duration
Must take apical pulse 1 minute before administration • Hold if under 60, contact MD • Blood levels needed
Digitalization is the administration of digitalis that is more than the maintenance dose • This raises the blood level quickly to therapeutic range • May also be called a loading dose
Example • Oral dose of digoxin 0.5-0.75 mg • 0.25-0.5 mg then given every 6-8 hours until desired blood level reached • Then maintenance dose: 0.125-0.5 mg daily
Digitalis toxicity: • GI distress: N/V, anorexia, and/or diarrhea (flu like symptoms) • May have excessive salivation and abdominal pain • Neurological: restless, irritable, lethargy, drowsiness, and/or confusion
May have vision changes, changes in color • May have halos, amblyopia and diplopia • Cardiac effects: development of arrhythmias (bradycardia, primary AV block)
Objective 10: identify factors which predispose digitalis toxicity
Contraindications • Toxicity predisposition: hypokalemia as cardiac muscles more sensitive to the glycosides • Renal impairment as 60-90% excreted by kidney • IV administration: rapid accumulation can occur
Treatment • Hold the drug • Use digoxin immune fab (Digibind) • Antigen-binding fragments combine with digoxin to neutralize its action
Lisinopril Animation Click here to view an animation on the topic of lisinopril.
Diuretics Prototype drug: furosemide (Lasix) Mechanism of action: to increase urine flow, reducing blood volume and cardiac workload Primary use: to reduce edema and pulmonary congestion Adverse effects: dehydration, electrolyte imbalance, hypotension, ototoxicity
Furosemide Animation Click here to view an animation on the topic of furosemide.
Cardiac Glycosides Prototype drug: digoxin (Lanoxin) Mechanism of action: to cause more forceful heartbeat, slower heart rate Primary use: to increase contractility or strength of myocardial contraction Adverse effects: neutropenia, dysrhythmias, digitalis toxicity
Beta-Adrenergic Blockers Prototype drug: Metoprolol (Lopressor, Troprol XL) Mechanism of action: block cardiac action of sympathetic nervous system to slow heart rate and B/P, reducing workload of heart Primary use: to reduce symptoms of heart failure and slow progression of disease Adverse effects: fluid retention, worsening of heart failure, fatigue, hypotension, bradycardia, heart block
Vasodilators Drugs: hydralazine (Apresoline); (isosorbide dinitrate (Isordil) Mechanism of action: to relax blood vessels Primary use: to lower blood pressure Used for clients who cannot take ACE inhibitors Adverse reactions: reflex tachycardia, orthostatic hypotension
Phosphodiesterase Inhibitors Prototype drug: milrinone (Primacor) Mechanism of action: to block enzyme phosphodiesterase in cardiac and smooth muscle Primary use: as short-term therapy for heart failure Adverse effects: hypokalemia, hypotension, ventricular dysrhythmias
Objective 11: describe the nursing responsibilities associated with administering cardiac glycosides preparations
Take apical pulse 1 full minute • Hold if under 60, over 100 in adults • Report any evidence of irregular rhythm • Observe for toxicity S/S • Monitor K+ if on diuretics • Encourage K+ rich foods
Teach client to take pulse • Teach S/S of toxicity • If hypothyroid, sensitive to digitalis • Draw blood levels periodically
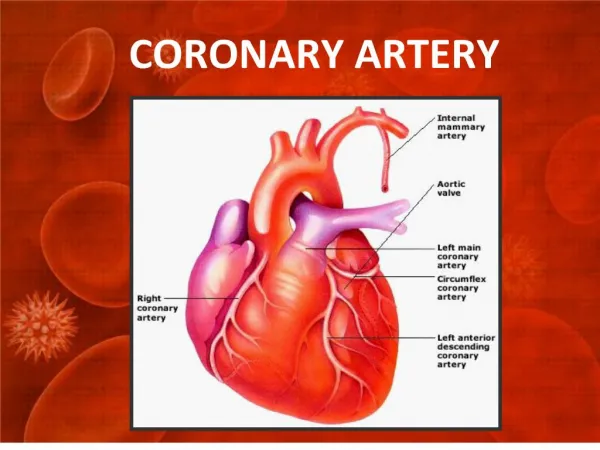
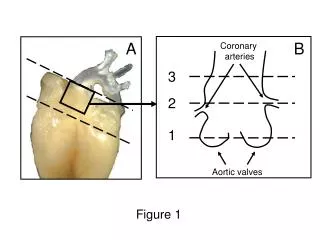
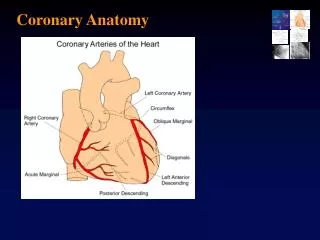
Angina • Atherosclerosis narrows heart’s vessels • Blood flow impeded • Demand exceeds supply = anginal pain