Anesthesia for Laparoscopic Surgery
410 likes | 2.79k Vues
Anesthesia for Laparoscopic Surgery 2007.4.13 R1 陳鈞婷 / 黃俊仁主任 Miller ’ s Anesthesia, 6th edition, Chapter 57 Benefits- reduce trauma,morbidity, mortality, hospital stay, health care costs, better maintenance of homeostasis

Anesthesia for Laparoscopic Surgery
E N D
Presentation Transcript
Anesthesia for Laparoscopic Surgery 2007.4.13 R1陳鈞婷/黃俊仁主任 Miller’s Anesthesia, 6th edition, Chapter 57
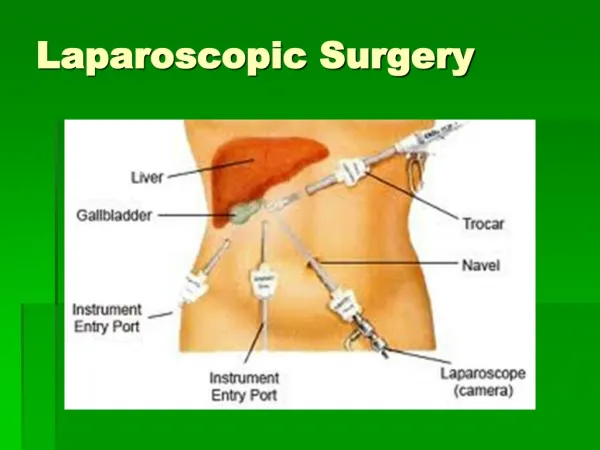
Benefits- reduce trauma,morbidity, mortality, hospital stay, health care costs, better maintenance of homeostasis • Complications- pathophysiologic changes, longer duration, unsuspected visceral injury, evaluating blood loss
Respiratory complications • CO2 pneumoperitoneum • CO2 subcutaneous emphysema • Pneumothorax • Endobronchial intubation • Gas embolism
Ventilatory Changes • ↓thoracopulmonary compliance (30-50%) in healthy, obese, ASA III/IV • ↓FRC due to diaphragm elevation • No change in physiologic dead space or shunt in healthy pat. when intra abdominal pressure(IAP) to 14mmHg and 10-200 tilt
PaCO2 plateau 15-30mins • PaCO2 depends on IAP • Local anesthesia – PaCO2 unchanged, ↑minute ventilation • IV general – compensatory hyperventilation insufficient due to respiratory depresssion and decreased compliance ∴ ↑PaCO2 • Post op :↑resp rate, PETCO2
Mean gradient(Δa-ETCO2) between PaCO2 and PETCO2 ↑more in ASA II/III than in ASA I • Eg.COPD, congenital heart disease • Lack of correlation between PaCO2 and PETCO2 in sick patients • Impaired CO2 excretion capacity • ABG recommended when hypercarbia suspected
Ventilatory changes • ASA I & II • Minute ventilation 100ml/kg/min • RR 12/min
Ventilatory changes • Open circles ASA I • Red circles ASA II-III
Causes of increased PaCO2 during laparoscopy • Absorption of CO2 from peritoneal cavity(main cause) • V/Q mismatch • Increased physiologic dead space, ↓alveolar ventilation • Abdominal distention • Position (eg. Steep tilt) • Controlled mechanical ventilation • Reduced cardiac output • Accentuated in sick patients • Increased metabolism(eg.insufficient anesthesia) • Depression of ventilation(eg.spontaneous breathing) • Accidental events :CO2 emphysema, Capnothorax, CO2 embolism, selective bronchial intubation
CO2 Subcutaneous Emphysema • Extraperitoneal insufflation • Eg. Inguinal hernia, renal surgery, pelvic lymphadenectomy • PaCO2 and PETCO2 increase after plateaued • Resolves after desufflation • Does not counterindicate tracheal extubation
Pneumothorax Pneumomediastinum Pneumopericardium • Embryonic remnants potential channels, Rt peritoneopleural ducts • Diaphragmatic defects, aortic and esophageal hiatus, pleural tears • Lung bullae • Capnothorax - ↓compliance, ↑airway pressure • Caution tension pneumothorax
Capnothorax Management(no lung trauma) • Stop N2O administraion • Adjust ventilator settings to correct hypoxemia • Apply PEEP • Reduce IAP as much as possible • Maintain close communication with surgeon • Avoid thoracocentesis unless necessary, spontaneous resolution after exsufflation
Pneumothorax from ruptured bullae • No PEEP • Thoracocentesis is required
Endobronchial Intubation • Cephalad displacement of diaphragm • Can occur in head up or down position • ↓SpO2 • ↑plateau airway pressure
Gas Embolism • CO2 more soluble than air, O2, N2O • Bicarbonate buffering, binding with Hb, plasma proteins, rapid elimination • Lethal dose >5x of air • Size and rate • Patent foramen ovale – emboli to coronary, brain • V/Q mismatch : physiologic dead space, hypoxia
Gas Embolism • <0.5ml/kg of air • ↑mean PAP • 2ml/kg of air • Tachycardia, arrhythmias, hypotension, ↑CVP, cyanosis, Rt heart strain • ↓PETCO2 • ↓cardiac output • ↑physiologic dead space • Initial increase in CO2 excretion
Treatment of CO2 embolism • Stop pneumoperitoneum • Steep head down and left lateral decubitus position • 100% O2 • Hyperventilation • Central venous line – aspirate gas • Foamy blood • External cardiac massage – break gas into small bubbles
Hemodynamic effects • Lower limb venous stasis • Literature : laparoscopy no ↑in DVT • ↓urine output and GFR • ↑cerebral blood flow • Arrhythmias • ↑Vagal tone (sudden peritoneum stretch, electrocoagulation of fallopian tubes) → bradycardia, arrhythmias, asystole • Vagal stimulation when low level anesthesia, B-blockers • Gas embolus
Positioning effects • Head down : ↑CVP and cardiac output • Affect patients with coronary artery disease • Elevation intraocular venous pressure(worsen acute glaucoma) • Increase risk of gas embolism • Atelectasis • Decreased FRC, total lung volume, compliance • Head up • ↓venous return →↓cardiac output and BP
Laparoscopy during Pregnancy • Risk of miscarriage, premature labour, fetal acidosis • Maternal PaCO2 maintained at normal level, fetal placental perfusion pressure, blood flow, pH then unaffected • Recommendations: • 2nd trimester, minimize preterm labor, adequate working room • Debatable use of tocolytics to arrest preterm labor • Open laparoscopy to avoid damaging uterus • Fetal monitoring with transvaginal ultrasonography • Mechanical ventilation to maintain physiologic maternal alkalosis
Anesthesia for laparoscopy • Positioned to prevent nerve injury • Tilt should not exceed 15-20 degrees • ET tube checked after position change • Monitors – BP,HR,EKG,CO2,SpO2 • ABG to correctly analyze PaCO2 • GA : safest technique compared to local, regional • Increase RR rather than tidal volume in COPD, spontaneous pneumothorax, bullous emphysema
Post op: hemodynamic changes(eg.↑SVR) outlasts the release of pneumoperitoneum • Increased O2 demand after laparoscopy • Higher RR and PETCO2 higher after laparoscopy • Prevention of nausea, vomiting