Thyroid and Parathyroid Disorders: Overview and Treatment Options
570 likes | 816 Vues
Learn about functional and structural disorders of the thyroid, thyroid physiology, evaluation of thyroid function, thyrotoxicosis, hyperthyroidism conditions like Graves Disease, toxic nodules, and treatment options like antithyroid drugs, radioactive iodine, and surgery.

Thyroid and Parathyroid Disorders: Overview and Treatment Options
E N D
Presentation Transcript
Thyroid and Parathyroid Disorders Sheila R. Gupta, M.D. May 1, 2011
Overview • Functional Disorders of the Thyroid • Hyperthyroidism • Hypothyroidism • Structural Disorders of the Thyroid • Thyroid Nodule • Goiter • Primary Hyperparathyroidism
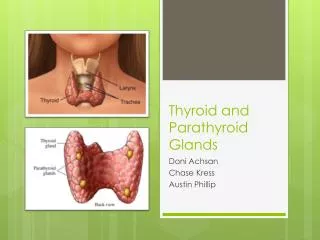
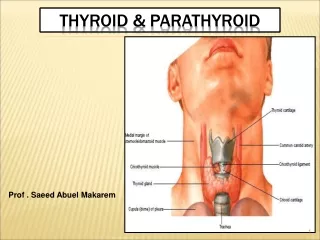
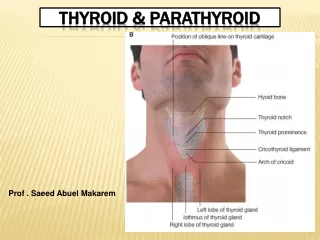
Thyroid Physiology • The thyroid gland primary produces T4 and only a small amount of T3 • Most T3 comes from peripheral conversion by 5’deiodinase enzymes • Free forms of T4 and T3 are biologically active
The Role of Iodine • Iodide is an essential component of thyroid hormone • Iodine deficiency is a worldwide health problem • Data from the NHANES study indicate generally adequate iodine intake in the United States • Pregnant and lactating women require 50-100% more daily iodine than the general population
Evaluation of Thyroid Function • TSH – most sensitive indicator of thyroid function • Free T4 - measurement by equilibrium dialysis remains the gold standard • T3 - measurement appropriate in hyperthyroidism to detect T3 toxicosis • Antibodies: • Anti-TPO antibodies: underlying autoimmune disorder with increased risk of hypothyroidism • TSI and TBII: pathognomonic for Graves disease • Thyroglobulin – tumor marker in patients with papillary or follicular thyroid cancer • Calcitonin – tumor marker for medullary thyroid cancer
Thyrotoxicosis • Thyroid Hormone Excess 1. Thyroiditis 2. TSH-secreting pituitary tumor 3. Thyroid hormone resistance 4. Exogenous T4/T3 5. Iodine load • Hyperthyroidism 1. Graves Disease 2. Toxic Multinodular goiter 3. Toxic Adenoma
Hyperthyroidism • Graves Disease • Toxic Multinodular Goiter • Toxic Adenoma
Patient has a low TSH. Next step? • Get a free T4 and T3 • If hyperthyroidism is confirmed by a low TSH, and elevated T4 and/or T3, get an I-123 thyroid uptake and scan • Thyroid uptake and scan – distinguishes between hyperthyroidism and thyroiditis
Graves Disease • Autoimmune process characterized by the production of antibodies against the TSH receptor. • When the antibodies bind to the TSH receptor they stimulate autonomous thyroid function • Risk factors: positive family history, other autoimmune conditions, recent severe stressors, tobacco use, viral exposures
Graves Disease: Physical Exam • Tachycardia • Elevated systolic blood pressure with a widened pulse pressure • Typically smooth enlarged thyroid gland with bruit • Stare due to lid retraction • Proptosis • Infiltrative dermopathy
Graves: Treatment • Antithyroidal drugs • 30-50% chance of remission after 1 year of therapy • Radioactive iodine ablation • Most common treatment in the United States • May take 6 months for full effects; consider re-dosing if still hyperthyroid after 6 months • Surgery • Typically reserved for patients with suspicious nodules, extremely large goiters, or moderate to severe ophthalmopathy
Antithyroid Drugs Methimazole Propylthiouracil (PTU) • First-line treatment • Once daily dosing • May cause elevated liver enzymes or agranulocytosis • Contraindicated in first trimester of pregnancy • Higher rate of serious adverse effects on the liver • May cause elevated aminotransferase levels or rarely severe hepatic necrosis • BID to TID dosing • May cause agranulocytosis • Preferred antithyroidal medication in first trimester of pregnancy
Graves Ophthalmopathy and RAI • Clinically significant ophthalmopathy occurs in 5-10% of patients with Graves disease • More common in smokers and those with family history • Radioactive iodine treatment has been associated with a worsening of ophthalmopathy • Consider prophylactic treatment with steroids
Toxic MultinodularGoiter and Toxic Nodule • Occurs due to a somatic mutation in the Gs-alpha subunit and the TSH receptor causing constitutive activation in one or more nodules, leading to autonomy of function and secondary thyrotoxicosis
Uptake and Scan in MNG and Toxic Nodule • Toxic Nodule: solitary “hot” nodule with suppression of the rest of the gland • Toxic MNG: patchy uptake with areas of both increased and decreased uptake • In toxic MNG, both an uptake and scan and thyroid ultrasound are useful in determining if there are any cold nodules that need FNA biopsy
Toxic Adenoma and MNG: Treatment • Antithyroidal drugs • Unlikely to achieve drug-free remission but will control thyroid hormone production • Radioactive Iodine • Definitive treatment • Hyperactive nodules take up iodine, and suppressed normal tissue receives minimal radiation exposure • Patients often return to euthyroidism without a need for thyroid hormone replacement • Surgery • Hemithyroidectomy versus total thyroidectomy
Destructive Thyroiditis • Subacute • de Quervain’s • Tender thyroid • Silent • Autoimmune • Generally painless • Postpartum • Occurs in 5% of pregnant women • Typically occurs within a few months of delivery
Drug-Induced Thyrotoxicosis • Lithium carbonate, interferon alfa, interleukin 2, iodinated contrast • Amiodarone • Type 1: Iodine-induced hyperthyroidism • Type 2: Destructive thyroiditis • Distinguish with ultrasound of the thyroid with Doppler imaging. High vascular flow pattern occurs in type 1 and low vascular flow pattern with type 2
Subclinical Hyperthyroidism • Suppressed TSH with concomitant T4 and T3 levels within normal limits • Symptoms are mild or patients may be asymptomatic • Potential negative effects of persistent mild thyrotoxicosis on the heart, bones, and CNS • Treat if the TSH is below 0.1 or if patients are symptomatic
Hypothyroidism • Clinical manifestations include:Fatigue, reduced endurance, weight gain, cold intolerance, constipation, impaired concentration and short-term memory, dry skin, edema, mood changes, depression, psychomotor retardation, muscle cramps, myalgia, and menstrual changes
Hypothyroidism: Physical Exam • Reduced basal temperature • Diastolic hypertension • Bradycardia Pallor • Dry and cold skin • Brittle hair • Hoarseness • Delayed recovery phase of deep tendon reflexes
Hypothyroidism: Diagnosis TSH, Free T4 Anti-TPO Antibodies
Brand name versus Generic • Position statement by the American Thyroid Association, American Association of Clinical Endocrinologists, and The Endocrine Society recommends that brand name is preferred to generic when it comes to thyroid hormone replacement
Armour and Cytomel • Armour - dessicated bovine thyroid containing a mixture of T4 and T3 • Cytomel - T3 alone • Thyrolar - T4 and T3 combination preparation • Multiple randomized trials have evaluated if hypothyroid patients may benefit from substitution of some T3 for T4 and no benefit or improvement in quality of life has been conclusively demonstrated
Optimal TSH Level • TSH normal range is very wide on most laboratory assays (0.5 – 5.0 uU/mL) • In patients with established hypothyroidism, the TSH target range is 1.0-2.5 uU/mL
Subclinical Hypothyroidism • Presence of an elevated TSH level with concomitant T4 and T3 levels within normal limits • Patients may also have mild elevations in total cholesterol, LDL cholesterol, and CRP, and increased risk for atherosclerosis and cardiac events • If patient is symptomatic, may treat to achieve a TSH of 1.0-2.5 uU/mL • Treatment is indicated if the TSH rises above 10 uU/mL
Thyroid Nodule • Nodules are common with aging and occur more frequently in women • Many thyroid nodules are found incidentally on imaging performed for other reasons • The majority of thyroid nodules are benign • 6-10% of nodules are malignant
Risk Factors for Thyroid Cancer • Personal history of any type of cancer • Family history of thyroid cancer • History of radiation to the face or neck Patients with increased cancer risk include those at extremes of age, male sex, rapid nodule growth, and hoarseness.
Thyroid Ultrasound • Any thyroid nodule greater than 1.0 cm in two different dimensions warrants fine needle aspiration biopsy • Some ultrasound characteristics are more concerning for malignancy: • Size greater than 3 cm • Speckled calcification within the nodule • High intravascular flow within the nodule’s center
When to get a CT or MRI • Substernal goiter • Cervical lymphadenopathy • Tracheal deviation
Thyroid Nodule Algorithm • Incidentally found a thyroid nodule on CT scan of the chest • Next step: TSH, free T4 • Next step: Thyroid ultrasound • If TSH is normal or high, and nodule is greater than 1.0 cm, then: • Next step: Thyroid FNA biopsy
Four Pathology Possibilities 1. Benign 2. Malignant 3. Follicular neoplasm/suspicious for malignancy 4. Insufficient
Benign Nodules • American Thyroid Association guidelines recommend a six month follow-up ultrasound after benign biopsy to assess for growth of the nodule • If nodule has grown by 50% by volume or has developed concerning ultrasound characteristics, consider repeat FNA • If no change, next imaging is in 3-5 years
Malignant Nodules • Malignant nodules are treated with near total thyroidectomy • High dose radioactive iodine ablation is often given after 3-4 weeks of withdrawal from thyroid hormone or with thyrogen stimulation • Six month follow-up ultrasound, whole body scan, and thyrogen-stimulated thyroglobulin levels are used for monitoring
Follicular Neoplasm Nodules • Total or near total thyroidectomy or lobectomy followed by completion thyroidectomy is indicated for suspicious nodules • 20% of nodules diagnosed as follicular neoplasm are malignant
Thyroid Hormone Suppression • Thyroid hormone suppression was previously used in an attempt to shrink thyroid nodules • Several randomized trials have evaluated the effect of thyroid hormone on nodule growth and the data are conflicting. • The 2009 American Thyroid Association Guidelines on Thyroid Nodules do not recommend routine thyroid hormone suppressive therapy for thyroid nodules
Goiter • Multinodular goiters occur more frequently with advancing age, low iodine intake, and Hashimoto’s disease • The cancer risk is similar for a thyroid gland with a solitary nodule or with multiple nodules • Nodule size and ultrasound characteristics are used to select the nodules to be biopsied
Large Multinodular Goiters • May have substernal extension • May have symptoms of dysphagia, hoarseness, dyspnea • Barium swallow, direct vocal cord visualization and/or spirometry with flow volume loops, and chest CT may be used to quantify the severity of any mass effect • Thyroidectomy indicated if symptomatic, malignancy suspected, or patient does not like cosmetic appearance
Nonthyroidal Illness • Euthyroid Sick Syndrome • T3 levels decline and reverse T3 rises • T4 levels remain relatively unchanged • TSH may be low, normal, or elevated • Thyroid hormone therapy not indicated • Thyroid hormone levels normalize 4-8 weeks after recovery from the illness
Parathyroid Disorders • Calcium levels are maintained by parathyroid hormone, vitamin D, and calcitonin • Calcium and phosphorus metabolism are closely related • Calcium is bound to plasma proteins such as albumin (40%), or exists as ionized calcium or bound to phosphorus and citrate (60%)
Actions of Parathyroid Hormone • Parathyroid cells sense decreases in the level of serum ionized calcium via the calcium-sensing receptor • PTH increases the serum calcium level within minutes by increasing renal and intestinal absorption of calcium and by rapidly mobilizing calcium and phosphate in bone • PTH also decreases renal phosphate reabsorption and increase urinary phosphate losses
Vitamin D • Vitamin D3 is derived from dietary sources and by skin exposure to ultraviolet light • UV light converts cholesterol precurosrs to vitamin D3 • Vitamin D3 is converted in the liver to 25-hydroxy vitamin D • 25-OH D undergoes 1 alpha hydroxylation in the proximal renal tubular cells to become 1,25-dihydroxy vitamin D
Primary Hyperparathyroidism • Diagnosis is established by an elevated serum calcium level and a PTH level that is elevated or inappropriately normal • Other lab findings: low serum phosphate, elevated urine calcium excretion, mild hyperchloremic metabolic acidosis
Causes of Primary Hyperparathyroidism • Solitary parathyroid adenoma: 80-85% • Double adenoma: 5% • Multigland parathyroid hyperplasia: 5-15% • Parathyroid carcinoma: 1%
Parathyroid Localization • Ultrasound • Technetium Tc99m sestamibi scintigraphy • MRI
Surgical Criteria for Asymptomatic Primary Hyperparathyroidism Established by the Third International Workshop in 2008 (NIH Workshop 2002): 1. Serum calcium greater than 1 mg/dL above the upper limit of normal 2. A creatinine clearance of less than 60 mL/min 3. Reduction in bone mineral density of the femoral neck, lumbar spine, or distal radius greater than -2.5 4. Age younger than 50 years 5. Patients for whom medical surveillance is not desirable or possible