Growth and Development of Bone
340 likes | 609 Vues
Growth and Development of Bone. Fall 2006. Introduction.

Growth and Development of Bone
E N D
Presentation Transcript
Growth and Development of Bone Fall 2006
Introduction • Bone (Latin: "os") is a type of hardendoskeletalconnective tissue found in many vertebrateanimals. Bone is the main tissue of body organs; organs that support body structures, protect internal organs, (in conjunction with muscles) facilitate movement; and are involved with cell formation, calcium metabolism, and mineral storage. The bones of an animal are, collectively, known as the skeleton. Bone has a different composition than cartilage, and both are derived from mesoderm. In common parlance, cartilage can also be called "bone", certainly when referring to animals that only have cartilage as hard connective tissue
Introduction • Bone is a relatively hard and lightweight composite material, formed mostly of calcium phosphate • Bone can be either compact or cancellous (spongy). Cortical (outer layer) bone is compact • Cortical bone accounts for 80% of the total bone mass of the adult skeleton
Introduction • Long bones are tubular in structure (e.g. the tibia). The central shaft of a long bone is called the diaphysis, and has a hollow middle—the medullary cavity filled with bone marrow. Surrounding the medullary cavity is a thin layer of cancellous bone that also contains marrow. The extremities of the bone are called the epiphyses and are mostly cancellous bone covered by a relatively thin layer of compact bone.
Introduction • Short bones (e.g. finger bones) have a similar structure to long bones, except that they are shorter. • Flat bones (e.g. the skull and ribs) consist of two layers of compact bone with a zone of cancellous bone sandwiched between them. • Irregular bones are bones which do not conform to any of the previous forms (e.g. vertebrae). • All bones consist of living cells embedded in a mineralised organic matrix that makes up the main bone material
Bone cells • Osteoblasts are typically viewed as bone forming cells. They are located near to the surface of bone and their functions are to make osteoid and manufacture hormones, such as prostaglandins, which act on bone itself.
Bone cells • Osteocytes originate from osteoblasts which have migrated into and become trapped and surrounded by bone matrix which they themselves produce. • The space which they occupy is known as a lacuna. • Their functions include to varying degrees: formation of bone, matrix maintenance and calcium homeostasis. • They possibly act as mechano-sensory receptors—regulating the bones' response to stress.
Bone cells • Osteoclasts are the cells responsible for bone resorption. Osteoclasts are large, multinucleated cells located on bone surfaces in what are called Howship's lacunae. • The process of bone resorption releases stored calcium into the systemic circulation and is an important process in regulating calcium balance. As bone formation actively fixes circulating calcium in its mineral form, resorption actively unfixes it thereby increasing circulating calcium levels. These processes occur in tandem at site-specific locations and are known as bone turnover or remodeling. Osteoblasts and osteoclasts, coupled together via paracrine cell signalling, are referred to as bone remodeling units.
Origin of Bone cells • Osteogenesis • Endochondral ossification • Requires a cartilaginous template • Intramembranous ossification • Lack of cartilaginous template • Axial Skeleton • Formed from sclerotome cells • Appendicular Skeleton • Formed from cells derived from the lateral plate mesoderm
Origin of cells • Osteoblasts come from mesenchymal cells and are directly involved in the bone matrix production • Osteocytes are mature osteoblasts are responsible for maintenance of the bone matrix • In adult bone, osteocytes out number osteoblasts
Origin of cells • Chondroblasts- form cartilage which is associated with bone required for bone growth • Osteoclasts are involved in bone resorption (breakdown) and remodeling. The number in adults is small • Bone lining cells – inactive cells found on the surface of the bone and may used as precursors for osteoblasts
Terms • Tendons- connective tissue that connects muscle to bone • Ligaments – connective tissue that connects bone to bone
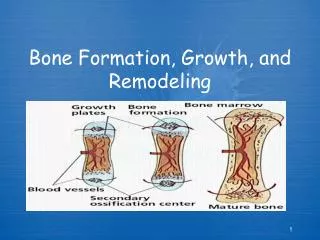
Endochondral Ossification • Occurs with the replacement of cartilage with bone • Both axial and appendicular skeletons develop cartilaginous structures prenatally and serves as a template for ossification • The cartilagenous matrix near the shaft of the bone begins to calcify as chondrocytes mature and enlarge • This calcification prevents nutrients from reaching the chondrocytes, thus they die, thus preventing new growth (ossification)
Endochondral Ossification • The perchondrium is converted into periosteum and ostioblasts become apparent in the inner layer of the periosteum. These form a layer of bone around the diaphysis. • Primary ossification center is established in the central portion of the shaft as a result of capillaries and osteblasts that migrate into that region
Endochondral Ossification • The calcified cartilage matrix in the center is broken down and action of the osteoblasts replaces the cartilage with new bone • Bone is formed from the center of ossification until the entire diaphysis is filled with spongy bone • As the bone grows, osteoclasts increase the inside diameter of the hollow central protion of the diaphysis so that the marrow cavity results
Endochondral Ossification • Secondary center of ossification occurs at each epiphysis • Osteoblasts in this area produce spongy bone that replaces the cartilage at the epiphyses. • A thin layer of articular cartilage to reduce the friction at joints (bone to bone)
Endochondral Ossification • The epiphyseal plate or growth plate is a thin region of cartilage between the diaphysis and epiphysis of long bones • Increased length of long bones involves action of both chondrocytes and osteoblasts at the growth plate • The chondrocytes closest to the epiphyseal side of the growth plate are a part of the reserve zone (stem cell zone)
Endochondral Ossification • Proliferating chondrocytes produce extracellular matrix such as collagens and proteoglycans • Mature chondrocytes eventually die and leave behind a calcified matrix which is replaced with bone via invading capillaries and osteoblasts • Chondroosseous junction is the region of growth between the cartilage and new bone
Endochondral Ossification • Degradation of the growth plate cartilage is important in allowing bone formation to occur at a normal rate • Growth plate turnover is the rate at which the condrocytes progress through the varying zones
Termination of long bone growth • The diaphysis of long bone will continue to lengthen as long as the rate of cartilage growth remains faster than the rate of osteoblast invasion at the growth plate – as long as it does not ossify • Cartilage growth stops or slows to a rate that allows it to be overcome with ossification – epiphyseal closure
Termination of long bone growth • Break joint in sheep – separation is at the distal end of the epiphyseal plate of the metacarpal bone • The distal end of the metacarpus is referred to as the spool joint
Intramembranous ossification • Increases in diameter of growing bone through appositional growth • Osteoblasts that differentiate from the periosteum deposit new bone matrix within the periosteum • Osteoblast activity is highest for those cells that surround the periosteal blood vessels
Intramembranous ossification • New osteons are produced as a result of the concentric deposition of bone that results from the action of osteoblasts and the formation of osteocytes • These new osteons contribute to compact bone and increase the overall outside diameter of the bone
Bone Resorption • While osteoblasts and osteocytes are adding new bone to the outer surface, osteoclasts are removing bone at th einner surface and enlarging the marrow cavity • Osteoclasts make contact with the bone through a region referred to as ruffled border and subsequently have the ability to degrade both inorganic and organic matrices of the bone
Bone Resorption • The degradation of the inorganic matrix is accomplished by solubilization of crystalline hydroxapatite crystals. • Osteoclasts appear to be capable of creating an acidic environment • The resulting decrease in pH in the local region is key to the solubilization process • This process results in the mobilization of minerals • Degradation of the organic matrix is accomplished with enzymes, including collagenase and proteinases
Bone Resorption • Types of marrow • Red marrow – chief blood cell forming organ of the adult and is found in spongy bone of the epiphysis of long bones and main bodies of ribs, sternum and vertebrae • Yellow marrow – composed mainly of adipose tissue and found in the medullary cavity of bones
Bone Remodeling • Osteoblasts form osteons (basic functional unit of compact bone) by osteogenesis whereas osteoclasts destroy osteons by resorption. • The balance between these two yields net bone deposition • As animals age, bone resorption may exceed formation and bone mass decreases
Bone Remodeling • Bone remodeling provides a mechanism for bone to adapt to new stresses especially heavily stressed bone that actually helps it become stronger • Remodeling is initiated through osteoclast activation to removal of bone matrix and is followed by osteoblast formation for the production of new bone. • Osteoblasts respond to the stress on bones and deposit additional bone in locations of stress to make bones stronger
Bone Remodeling • Increased force of muscles will result in increased bone growth where tendons connect to bones • The amount of stress is closely related to the degree of mineralization and porosity
Factors affecting bone growth and remodeling • A lot of bone remodeling is a result of hormonal action. • Hormones involved in bone growth and remodeling is PTH and Calcitonin • Calcitonin is released by the thyroid gland that decreases osteoclasts yielding decreased mobilization of calcium from bone and decreasing blood calcium concentrations
Factors affecting bone growth and remodeling • PTH acts on bone, kidney, and gastrointestinal tract to increase blood calcium • Action on bone includes an increase in osteoclast activity • This is mediated through signals from osteoblasts and osteocytes and often mobilization of calcium out of bone via osteoclasts • Also, PTH regulates phosphorus metabolism
Factors affecting bone growth and remodeling • Other hormones that regulate bone growth and remodeling are testosterone and estrogen • Both estrogen and testosterone hasten ossification and have an effect on epiphyseal closure • As a result, castration yields longer bones (longer, taller animals) because of slower closure processes • Estrogens are more effective in mediating closure of the growth plate than testosterone, thus females are smaller statured than males