Abdominal and Genitourinary Trauma
230 likes | 1.14k Vues
Abdominal and Genitourinary Trauma. Chapter 35. Objectives. Review anatomy of the abdominal cavity Discuss Abdominal Trauma Discuss Genital Trauma. Abdominal cavity. Peritoneum – 2 layer sheath like membrane Visceral peritoneum – innermost lining

Abdominal and Genitourinary Trauma
E N D
Presentation Transcript
Abdominal and Genitourinary Trauma Chapter 35
Objectives • Review anatomy of the abdominal cavity • Discuss Abdominal Trauma • Discuss Genital Trauma
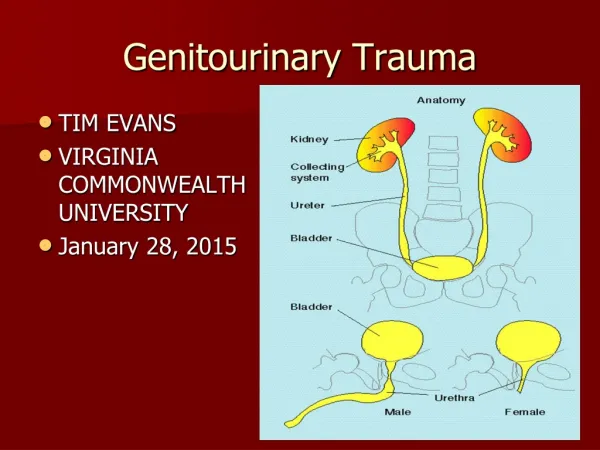
Abdominal cavity • Peritoneum – 2 layer sheath like membrane • Visceral peritoneum – innermost lining • Parietal peritoneum – outer lining that adheres to the walls of the abdominal cavity • Peritoneal cavity – the potential space between the visceral and parietal peritonea • Retroperitoneal cavity – Posterior space
Hollow Organs • Stomach • Gall bladder • Urinary bladder • Ureters • Internal urethra • Fallopian tubes • Small intestines • Large intestines
Solid Organs • Liver • Spleen • Pancreas • Kidneys
Vascular and Additional Structures Vascular Structures • Abdominal aorta • Inferior Vena Cava Additional structures • Diaphragm • Abdominal wall
Abdominal Injuries • Blunt or penetrating trauma can cause abdominal injuries • MOI are similar to those of chest injury • Blunt trauma is especially lethal due to the large number of organs present • Open abdominal injuries result from penetrating trauma such as gunshot, stabbing or other hard sharp objects • Gunshot wounds, always examine for an exit wound • Open wounds are easier to see, but may be less dangerous than closed wounds • Always maintain suspicion of the existence of a closed abdominal injury
Assessment based approach Scene size-up • BSI • Scan scene for MOI • Ask police/bystanders what happened, especially if gunshots were heard • Attempt to determine the following, for vehicle collisions; • Type of vehicle • Approximate speed • Type of collision/point of impact • Was patient driver, passenger, or pedestrian • Where was patient found, in what position • Was patient ejected? • Impact marks on windshield, steering wheel, and dashboard • Was patient wearing a seatbelt?
Primary Assessment Form a general impression • Is patient lying still with knees flexed? • Is patient moaning and complaining of severe pain? • Spinal injury suspected, in-line stabilization • Ensure open airway • Check for vomit, prepare for suctioning • Oxygen via NRB @ 15 lpm, if adequate respirations • Ventilation, if inadequate • Assess circulation and look for signs of shock and abdominal injury • Weak or absent radial pulse • Abnormally rapid heart rate • Moist, pale, cool skin • If signs are present, patient is priority to immediate transport
Secondary Assessment • Consider complaints and MOI • Expose the entire body and perform a rapid secondary assessment: head, neck, and chest first • Apply cervical immobilization, if spinal injury suspected • Inspect abdomen for open wounds, distension • Inspect around the navel and flanks for discoloration and bruising • Look for bruising in lower abdomen • Inspect and provide emergency care for abdominal evisceration
Secondary Assessment • Palpate abdomen, noting tenderness, masses or signs of pain • Assess extremities for injuries; check and compare pulses • Assess motor and sensory function • Log roll the patient and inspect back and lumbar region; log roll onto backboard if spinal injury is suspected • Assess baseline vitals • Obtain history; if patient is unresponsive, ask bystanders
Secondary Assessment Be alert for the following signs and symptoms of abdominal injury • Contusions, abrasions, lacerations, punctures, or other signs of blunt or penetrating trauma • Pain that continues to get worse • Tenderness on palpation to areas besides injury site • Rigid abdominal muscles • Patient has drawn up legs to his chest to reduce pain • Distended abdomen • Discoloration around the navel or the flank (late sign) • Rapid, shallow breathing • Signs of hemorrhagic shock • Decreasing blood pressure, narrowing pulse pressure, increasing heart rate, increasing respiratory rate • Nausea/vomiting • Abdominal cramping • Pain that radiates to either shoulder • Weakness
General emergency care – abdominal trauma • Maintain open airway and appropriate spinal protection • Oxygen therapy • Reassess breathing status • Treat for shock if symptoms apparent • Control external bleeding • Supine position with knees flexed • Stabilize an impaled object • Apply PASG if appropriate • Transport quickly
Emergency care - Evisceration • Expose the wound • Position patient supine with knees flexed • Prepare clean, sterile dressing • Cover the moist dressing with an occlusive dressing • Administer high-flow, high-concentration oxygen • Treat for shock • Reassess for effectiveness • Assess for further deterioration • Reassess vital signs
Genital Trauma Injuries to male genitalia • Lacerations, abrasions, avulsions, penetrations, amputations, contusions • Usually excruciatingly painful and causes great concern for the patient • Penis is very vascular • Treat as soft-tissue injury; apply direct pressure and cold compress • Wrap avulsed parts in sterile, moist dressing; place on ice; and transport with patient • Oxygen via NRB @ 15 lpm • Assess for signs of shock and transport
Injuries to Female genitalia Include straddle injuries, sexual assault, blunt trauma, abortion attempts, lacerations after childbirth, and foreign bodies inserted into vagina • Usually produces excruciating pain and causes concern for the patient • Area is highly vascular • Apply direct pressure to any bleeding; use moist compress • Never pack or place dressings inside vagina • Assess for shock • Oxygen via NRB @ 15 lpm • Transport
Rectal Injury Weightlifter in competition. (prolapse) How would you treat and package for transport?