The Urinary System
850 likes | 986 Vues
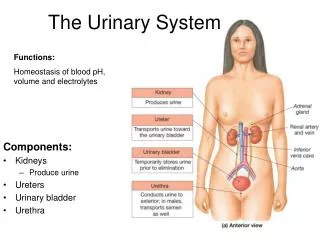
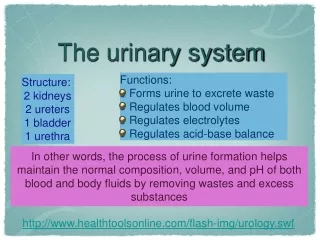
25. The Urinary System. Kidney Functions. Regulate chemical composition of body fluids Eliminates waste Controls composition of bloods – ion levels and concentration Help maintain PCO2 & acid/base balance [pH] Help regulate blood pressure by secreting renin [ renin-angiotensin system].

The Urinary System
E N D
Presentation Transcript
25 The Urinary System
Kidney Functions • Regulate chemical composition of body fluids • Eliminates waste • Controls composition of bloods – ion levels and concentration • Help maintain PCO2 & acid/base balance [pH] • Help regulate blood pressure by secreting renin [renin-angiotensin system]
Kidney Functions • Contribute to metabolism • detoxify free radicals and drugs [with peroxisomes] • gluconeogenesis [during fasting] • produce erythropoietin – stimulates red blood cell production • activation of vitamin D [as calcitrol]
NITROGENOUS WASTES • Metabolic waste – waste substance produced by the body [often lethal] • 50% of N containing waste is urea [from protein – aa NH2 ammonia urea [by liver] • Uric acid – from nucleic acids • Creatinine – from creatine phosphate
NITROGENOUS WASTES • BUN – typical = 10-20 mg/dL Too high = azotemia [renal insufficiency] • Plasma creatinine increase above 1.5 mg/dL with decreased filtration normal = 0.6-1.2 mg/dL
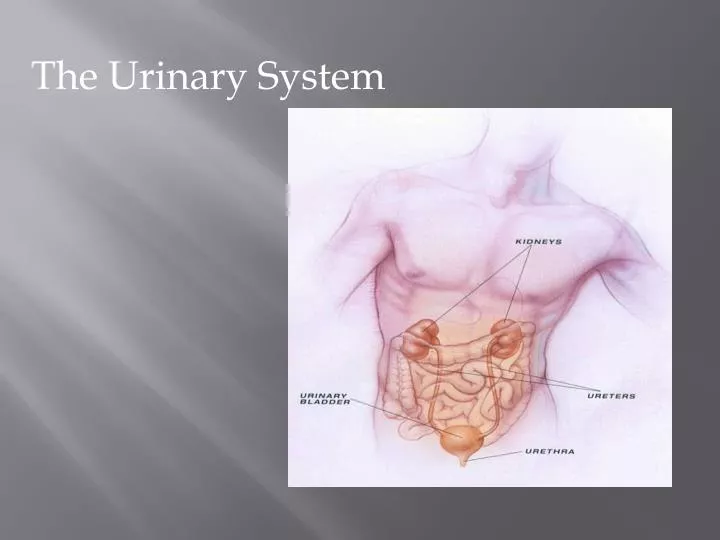
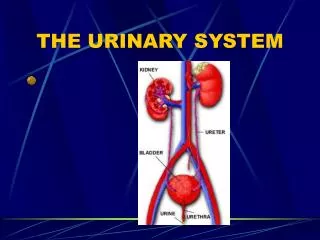
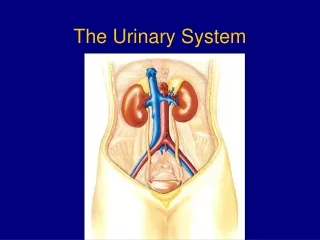
Kidney Location and External Anatomy • Retroperitoneal in the superior lumbar region. • Extend from twelfth thoracic to third lumbar vertebra. • Right kidney is lower than left because it is crowded by the liver.
Layers of Tissue Supporting the Kidney • Renal fascia – outer layer of dense fibrous connective tissue that anchors the kidney to abdominal wall. • Adipose capsule – shock absorbing. • Renal capsule – fibrous cover that prevents kidney infection.
Internal Anatomy • Cortex –outer - cortical zone and juxtamedullary zone • Medulla – renal pyramids [8-18] • Renal papillae – narrow ends of pyramids • Renal columns – between pyramids
Internal Anatomy • Urine Flow – formed in nephrons papillary ducts minor calyx major calyx renal pelvis
Blood and Nerve Supply • ~ one-fourth (1200 ml) of systemic cardiac output flows through the kidneys each minute. • Arterial flow into venous flow out of the kidneys follow similar paths. Figure 25.3c
Blood and Nerve Supply • Renal Arteries segmental arteries interlobar arteries arcuate arteries cortical radial arteries afferent arterioles • Efferent arterioles also form vasa recta with deep juxtamedulary nephrons • Venules cortical radial veins arcuate veins interlobar veins segmental veins renal veins inferior vena cava Figure 25.3c
Blood and Nerve Supply NERVE SUPPLY - • Renal plexus of sympathetic division of ANS – to afferent & efferent arterioles [vasomotor nerves] - regulate flow and pressure Figure 25.3c
The Nephron • Nephrons are the structural & functional units that form urine, consisting of: • Renal Corpuscle – glomerulus + Bowman’s capsule • Renal Tubule - PCT, loop of Henle, DCT
Histology of Nephron – Corpuscle BOWMAN”S CAPSULE • Parietal layer – simple squamous epithelium. • Capsular space. • Visceral layer consists of modified, branching epithelial podocytes.
Histology of Nephron – Corpuscle • Functions – pressure filtration of blood – water and small solutes leave blood • vascular pole - blood in • urinary pole -urine out
VP UP
Histology of Renal Tubule • Proximal convoluted tubule (PCT) – cuboidal epithelium with microvilli & mitochondria
Histology of Renal Tubule Loop of Henle [nephron loop]: • Descending limb [thin] simple squamous epithelium – permeable to water [out], urea [in]; thick walls • Ascending limb [thick] – cuboidal to low columnar epithelium; thick at top, then thin
Connecting Tubules Distal convoluted tubule (DCT): • Principal cells: • Cuboidal cells without microvilli. • Help maintain water & salt balance.
Collecting Ducts • Collecting Ducts - drains several DCT's • Combine to form papillary ducts calyces • Cuboidal epithelium, then columnar
Nephrons All nephrons begin in the cortex. Where the loop of Henle reaches to determines type • Juxtamedullary nephrons: • Have loops of Henle that deeply penetrate medulla. • Cortical nephrons – 85% of nephrons: • Have loops of Henle that only slightly penetrate medulla.
Nephrons Figure 25.5b
Glomerular Filtration General • Glomerular filtrate - from plasma but with no protein • Tubular fluid - from PCT through DCT
Filtration Membrane • Endothelium of glomerulus – open pores [fenestrations] – 70-90 nm diameter everything but cells and platelets pass through • Basal lamina [basement membrane] of glomerulus – serves as dialysis membrane –blocks large plasma proteins
Filtration Membrane • Filtration slits - Endothelium of visceral layer of glomerular capsule – podocytes form filtration slits [spaces between pedicels] – negatively charged - repel anions - 30 nm slit width
Net Filtration Pressure (NFP) • Glomerulus blood filtering depends on 3 main pressures –1 promotes, 2 oppose • Blood Hydrostatic Pressure [HPG] – about 60 torr – forces fluid out of capillaries • Capsular Hydrostatic Pressure [HPC] – about -18 torr – opposes –from fluid already in capsular space
Net Filtration Pressure (NFP) • Colloidal Osmotic Pressure of blood [OPC] about -32 torr – opposes • NFP = HPG – [HPC +OPC] = 55 – [15- 30]] = about 10 torr outward • The positive pressure moves fluid out of the glomerulus into Bowman’s capsule.
Net Filtration Pressure (NFP) • Pressure remains high throughout length so filtration continues. Especially sensitive to hypertension
Glomerular Filtration Rate (GFR) • Amount of filtrate formed in all areas of the renal corpuscles of both kidneys every minute • Directly related to pressures that determine NFP • Adult rate is about 125 mL/min – 180L/day [males]
Regulation of Glomerular Filtration • If the GFR is too high: • Needed substances cannot be reabsorbed quickly enough and are lost in the urine. • If the GFR is too low: • Everything is reabsorbed, including wastes that are normally disposed of.
Regulation of Glomerular Filtration • Three mechanisms control GFR: • Renal autoregulation (intrinsic system); • Neural controls; • Hormonal mechanisms (renin-angiotensin system).
Regulation of Glomerular Filtration • Renal Autoregulation of GFR - blood flow autoadjustment • Myogenic Mechanism – Smooth muscle contracts when stretched reduces blood flow which reduces pressure downstream.
Regulation of Glomerular Filtration • Tubuloglomerular feedback – negative feedback mechanism using the • Juxtaglomerular apparatus [respond to NaCl concentration] • juxtaglomerular cells - smooth muscle fibers of afferent arterioles – mechanoreceptors - dilate or constrict with pressure change & secrete renin.
Regulation of Glomerular Filtration • macula densa- chemoreceptors – at end of ascending limb tall crowded cells that monitor Na+ and Cl- concentration
Juxtaglomerular Apparatus (JGA) DC Muller, Johns Hopkins School of Medicine
Regulation of Glomerular Filtration • Neural Regulation – sympathetic • Norepinephrine causes vasoconstriction • Affects smooth muscles of vessels – low input dilation, high constriction
Regulation of Glomerular Filtration • Renin-angiotensin II pathway- JG cells release renin in response to • 1 – decreased delivery of fluid and NaCl to macula densa • 2 – decreased stretching of JG cells • 3 – increased rate of stimulation by renal sympathetic nerves
Regulation of Glomerular Filtration Angiotensin II is the active hormone that • produces constriction of arterioles to increase GBHP and raise GFR • stimulates secretion of aldosterone, which enhances reabsorption of Na+ [and water] by principal cells in collecting ducts
Regulation of Glomerular Filtration • stimulates the thirst center of the hypothalamus • stimulates release of ADH which increases water reabsorption increase in blood volume higher BP
Capillary Beds of the Nephron • Every nephron has 2 capillary beds: Glomerulus & Peritubular • Each glomerulus is: • Fed by an afferent arteriole • Drained by an efferent arteriole
Capillary Beds • Peritubular beds are low-pressure, porous capillaries. • Vasa recta – long, straight efferent arterioles of juxtamedullary nephrons.
Tubular Reabsorption • 99% of materials move from filtrate back into peritubular capillaries or vasa recta • Solutes are reabsorbed by active or passive transport • Water is reabsorbed by osmosis = facultative water reabsorption • Small peptides and proteins are reabsorbed by pinocytosis