HEMORRHAGIC
480 likes | 719 Vues
HEMORRHAGIC. ALTERNATIVE NAMES. Hemorrhagic dengue Dengue shock syndrome H - Fever Breakbone fever dandy fever.

HEMORRHAGIC
E N D
Presentation Transcript
ALTERNATIVE NAMES Hemorrhagic dengue Dengue shock syndrome H - Fever Breakbone fever dandy fever
Dengue Hemorrhagic Fever is an acute infectious viral disease usually affecting infants and young children. This disease used to be called break-bone fever because it sometimes causes severe joint and muscle pain that feels like bones are breaking. is a severe, potentially deadly infection spread by certain species of mosquitoes (Aedes aegypti). Philippine Hemorrhagic Fever was first reported in 1953. in 1958, hemorrhagic fever became a notifiable disease in the country and was later reclassified as Dengue Hemorrhagic Fever.
Dengue (pronounced DENG-gay) can affect anyone but tends to be more severe in people with compromised immune systems. Because it is caused by one of four serotypes of virus, it is possible to get dengue fever multiple times. However, an attack of dengue produces immunity for a lifetime to that particular serotype to which the patient was exposed.
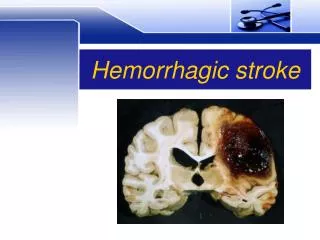
Dengue Hemorrhagic Fever is a more severe form of the viral illness. Symptoms include headache, fever, rash, and evidence of hemorrhage in the body. Petechiae (small red or purple splotches or blisters under the skin), bleeding in the nose or gums, black stools, or easy bruising are all possible signs of hemorrhage. This form of dengue fever can be life-threatening and can progress to the most severe form of the illness, dengue shock syndrome.
How is dengue fever contracted? • The virus is contracted from the bite of a striped Aedes aegypti mosquito that has previously bitten an infected person. The mosquito flourishes during rainy seasons but can breed in water-filled flower pots, plastic bags, and cans year-round. One mosquito bite can cause the disease. • The virus is not contagious and cannot be spread directly from person to person. There must be a person-to-mosquito-to-another-person pathway.
An acute febrile infection of sudden onset with clinical manifestation of 3 stages:
First 4 days – Febrile or Invasive Stage high fever Abdominal pain and headache Later flushing which may accompanied by vomiting, conjunctival infection and epistaxis
4th-7th days – Toxic or Hemorrhagic Stage Lowering of temperature Severe abdominal pain Vomiting and frequent bleeding from gastrointestinal tract in the form of hematemesis or melena Unstable BP Narrow pulse pressure shock
7th-10th day – Convalescent or Recovery stage Generalized flushing with intervening areas of blanching appetite regained Blood pressure already stable
Severe, frank type – with flushing, sudden high fever, severe hemorrhage, followed by sudden drop of temperature, shock and terminating in recovery or death. Moderate – with high fever, but less hemorrhage, no shock Mild – with slight fever, with or without petechial hemorrhage but epidemiologically related to typical cases usually discovered in the course of investigation of typical cases.
Flavivirus, Dengue Virus Types 1, 2, 3, & 4 Chikungunya Virus
Vector mosquito Aedis Aegypti , Aedis albopictus, The infected person
INCUBATION PERIOD UNCERTAIN. Probably 6 days to 1 week PERIOD OF COMMUNICABILITY Unknown. Presumed to be on the first week of illness when virus is still present in the blood.
SUSCEPTIBILITY, RESISTANCE AND OCCURRENCE All persons are susceptible. Bothe sexes are equally affected. Age groups predominantly affected are the preschool age and school age. Adults and infants are not exempted. Peak age affected 5-9 years. Occurrence is sporadic through out the year. Epidemic usually occur during the rainy seasons June – November. Peak months are September and October. Occurs wherever vector mosquito exists. Susceptibility is universal. Acquired immunity may be temporary but usually permanent.
Physical Examination may reveal the following: Low BP A weak, rapid pulse Rash Red eyes Red throat Swollen glands Enlarged liver (hepatomegaly)
Test may iclude the following: Hematocrit Platelet count Electrolytes Coagulation studies Liver enzymes Blood gases Torniquet test (causes petechiae below the torniquet) X-ray of the chest (may demonstrate pleural effusion) Serologic studies (demonstrate antibodies to Dengue viruses) Serum studies from samples taken during acute illness and convalescence (High in titer to Dengue antigen)
Most people who develop DHF recover completely within 2 weeks. Some, however, may go through several weeks to months of feeling tired and/or depressed. Others develop severe bleeding problems. This complication, DHF, is a serious illness which can lead to shock (very low BP) and is sometimes fatal especially to children and young adults.
Other complications are the following: Shock Encephalopathy Residual brain damage Seizures Liver damage
Supportive and symptomatic treatment should be provided For fever, give paracetamol for muscle pains. For headache, give analgesic. DON’T give ASPIRIN. Rapid replacement of body fluids is trhe most important treatment Includes intensive monitoring and follow-up. Give ORESOL to replace fluid as in moderate dehydration at 75 ml/kg in 4-6 hours or up to 2-3L in adults. Continue ORS intake until patient’s condition improves.
The infected individual, contacts and environment: Recognition of the disease. Isolation of patient (screening or sleeping under the mosquito net) Epidemiological investigation Case finding and reporting Health Education
Eliminate the vector by: Changing water and scrubbing sides of lower vases once a week. Destroy breeding places of mosquito by cleaning surroundings Proper disposal of rubber tires, empty bottles and cans. Keep water containers covered. Avoid too many hanging clothes inside the house. Residual spraying with insecticides
Search and destroy Self protection Seek early consultation Say no to indiscriminate fogging
Report immediately to the municipal Health Office any known case outbreak. Refer immediately to the nearest hospital, cases that exhibit symptoms of hemorrhage from any part of the body no matter how slight. Conduct a strong health education program directed towards environmental sanitation particularly destruction of all known breeding places of mosquitoes. Assist in the diagnosis of suspect based on the s/sx. For those without signs of hemorrhage, the nurse may do the “torniquet” test. Conduct epidemiologic investigations as a means of contacting families, case finding and individual as well as community health education
For hemorrhage – keep the px at rest during bleeding episodes. For nose bleeding, maintain an elevated position of trunk and promote vasoconstriction in nasal mucosa membrane through an ice bag over the forehead. For melena, ice bag over the abdomen. Avoid unnecessary movement. If transfusion is given, support the patient during the therapy. Observe signs of deterioration (shock) such as low pulse, cold clammy perspiration, prostration..
2. For shock – prevention is the best treatment. Dorsal recumbent position facilitates circulation. Adequate preparation of the patient, mentally and physically prevents occurrence of shock. Provision of warmth-through lightweight covers (overheating causes vasodilation which aggravates bleeding). 3. Diet – low fat, low fiber, non-irritating, non-carbonated. Noodle soup may be given.
In medicine and biology, transmission is the passing of a communicable disease from an infected host individual or group to a conspecific individual or group, regardless of whether the other individual was previously infected. • Sometimes transmission can specifically mean infection of a previously uninfected host. • The term usually refers to the transmission of microorganisms directly from one person to another by one or more of the following means: • droplet contact – coughing or sneezing on another person
direct physical contact – touching an infected person, including sexual contact • indirect physical contact – usually by touching soil contamination or a contaminated surface • airborne transmission – if the microorganism can remain in the air for long periods • fecal-oral transmission – usually from contaminated food or water sources
Incubation period • is the time elapsed between exposure to a pathogenicorganism, a chemical or radiation, and when symptoms and signs are first apparent. The period may be as short as minutes to as long as thirty years in the case of variant Creutzfeldt–Jakob disease.
Period of Communicability • the time during which the patient is infectious to others.
Infectious • Capable of causing infection. • Caused by or capable of being transmitted by infection. • Caused by a pathogenic microorganism or agent.
Contagious • Capable of being transmitted from one person to another by direct or indirect contact. • Capable of transmitting disease; carrying a disease.