The Complement System
230 likes | 612 Vues
The Complement System. Andrew E Thompson MD FRCPC Fellow in Rheumatology University of British Columbia. Overview. The complement system is part of the innate immune system (vs adaptive)

The Complement System
E N D
Presentation Transcript
The Complement System Andrew E Thompson MD FRCPC Fellow in Rheumatology University of British Columbia
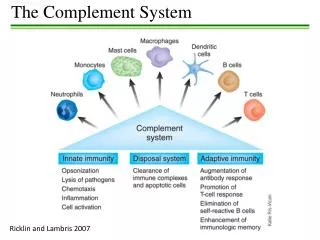
Overview • The complement system is part of the innate immune system (vs adaptive) • It is named “complement system” because it was first identified as a heat-labile component of serum that “complemented” antibodies in the killing of bacteria • It is now known that it consists of over 30 proteins and contributes 3 g/L to overall serum protein quantities
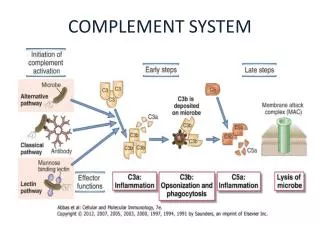
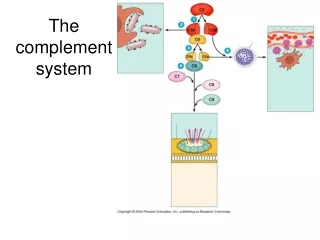
“Classical” Pathway • Begins with antibody binding to a cell surface and ends with the lysis of the cell • The proteins in this pathway are named C1-C9 (the order they were discovered and not the order of the reaction) • When complement is activated it is split into two parts • a – smaller of the two • B – larger part and usually the active part (except with factor 2) • Remember 3 Key Words • ACTIVATION • AMPLIFICATION • ATTACK
“Classical Pathway” • ACTIVATION • C1q portion of C1 attaches to the Fc portion of an antibody • Only IgG and IgM can activate complement • Once activated C1s is eventually cleaved which activates C4 and C2 • C4b & C2a come together to form the C4b2a which is the C3 convertase • C3 convertase activates C3 to C3a and C3b
“Classical Pathway” • ACTIVATION • C3a binds to receptors on basophils and mast cells triggering them to release there vasoactive compounds (enhances vasodilation and vasopermeability) • C3a is called an anaphylatoxin • C3b serves as an opsonin which facilitates immune complex clearance
“Classical Pathway” • AMPLIFICATION • Each C1s creates many C4b and C2b fragments • Each C4bC2a creates many C3b (activated C3) • Each C3b goes on to create many Membrane Attack Complexes • Example • 1 C1S makes 100 C4bC2b • 100 C4bC2b makes 10,000 C3b • 10,000 C3b makes 1,000,000 MAC
“Classical Pathway” • ATTACK • Most C3b serves an opsonin function • Some C3b binds to C4bC2a to form the C5 convertase C4bC2aC3b • C5 convertase cleaves C5 leading to the formation of the Membrane attack Complex (C5-C6-C7-C8-C9) • The MAC “punches holes” in cell walls resulting in lysis
C3 C3b 4b C4 C3a 2b C1q C2 4a 2a C5 C5a C5b C7 C6 C8 C3a binds to receptors on basophils and mast cells triggering them to release there vasoactive compounds (enhances vasodilation and vasopermeability) - ANAPHYLATOXIN • C5a is a: • Potent anaphylatoxin • Chemoattractant for neutrophils C3-convertase C5-Convertase C9 Classical Pathway
“Alternative Pathway” • Requires no specific recognition of antigen in order to cause activation
“Alternative Pathway” • ACTIVATION • Spontaneous conversion from C3 to C3b occurs in body • Normally, C3b is very short lived and quickly inactivated by proteins on the surface of the body’s own cell walls • However, bacteria or other foreign material may lack these surface proteins allowing C3b to bind and stay active
“Alternative Pathway” • AMPLIFICATION • Factor B binds to C3b • Factor B is then cleaved by factor D into Ba and Bb • C3bBb remains which acts as a C3 convertase (C3 C3a and C3b) • C3bBbC3b is formed which acts as a C5 convertase
“Alternative Pathway” • ATTACK • C5 is cleaved to C5a and C5b • C5b then starts the assembly of the Membrane Attack Complex
C3 C3 C3b C3b C3a C3a Bb Ba C5 D B C5a C5b C7 C6 C8 Anaphylatoxin Alternative Pathway C3-Convertase C5-Convertase C9
Summary - Activation • Complement can be activated by the binding of antibody (Classical) or by the adherance of C3b to foreign material (Alternative) • The two pathways converge at the formation of the C5 convertase (C4b2a3b or C3bBbC3b) • The final common pathway is the formation of the membrane attack complex
Summary - Function • Opsonization – C3b • Chemotaxis – C5a (attracts neutrophils) • Increases vasodilation & permeability of capillary beds via mast cell and basophil activation – C3a & C5a (Anaphylatoxins) • Cellular Lysis via the MAC
Laboratory Measures • C3 – Quantitative measure (nephelometry) • C4 – Quantitative measure (nephelometry) • CH50 • Functional assay of entire Classical Pathway • Measures the ability of the patients serum to lyse 50% of a standard suspension of sheep erythrocytes coated with rabbit antibody • A low CH50 suggests either • CONSUMPTION OF COMPLEMENT COMPONENTS • DEFICIENCY OF COMPLEMENT COMPONENTS • AH50
The Role of Complement in the Rheumatic Diseases • The Double Edged Sword! • Needed for proper handling of immune complexes • Also mediates tissue damage, especially in the setting of autoantibodies and excessive immune complex formation • Just as the complement system can destroy a microbe, it can lyse and erythrocyte, phagocytose a platelet, or disrupt a basement membrane
Autoimmunity and InheritedComplement Deficiencies • Inherited deficiencies of complement components can result in autoimmunity, especially SLE • C1q deficiency – 90% have SLE • C4 deficiency – 75-80% have SLE • C2 deficiency – 10-40% have SLE • Early age of onset, prominent cutaneous manifestations, and presence of anti-Ro antibodies are features suggestive of a complement deficiency
Autoimmunity and Inherited Complement Deficiencies QUIZ TIME • Q: Dendritic Cells present antigen with MHC Class I or MHC Class II? • A: MHC Class II – It is an APC (antigen presenting cell) • Q: MHC Class II molecules present antigen derived from intracellular or extracellular processes? • A: Extra-cellular (e.g. apoptotic cells) • Q: MHC Class II molecules stimulate CD4 or CD8 cells • A: CD4 (IIx4=8, Ix8=8) • Q: In this scenario with the APC being a dendritic cell – the CD4 T-lymphocyte it interacts with is a Th1 or Th2? • A: Th1 is chiefly involved in cellular mediated immunity and Th2 is chiefly involved in humoral mediated immunity – Th2 • How does SLE form with complement deficiencies? • Failure to clear autoantigens (apoptotic cells) • Immature dendritic cells uptake the antigen in the presence of inflammatory cytokines causing them to mature into antigen presenting dendritic cells – Presents to T-Cell • Autoreactive B-Cells take up antigen from apoptotic cells and (with the help CD4+ Th2-Cells) transform into plasma cells that secrete autoantibody
Indirect Laboratory uses of Complement – Detection of Immune Complexes • C1q binding Assay • Normally C1q has a very weak affinity for monomeric IgG and IgM • When IgG or IgM are part of an immune complex the Fc portion undergoes a conformational change • This results in a much higher affinity for C1q • This test is an ELISA which looks for immune complexes in a patients serum capable of binding C1q
Indirect Laboratory uses of Complement – Detection of Immune Complexes • Raji Cell Preparation • Raji cells are a human lymphoblastoid cell derived from a patient with Burkitt’s lymphoma • They are unique because • They have surface receptors for C1q, C3b, C3bi, and C3d • Lack of surface immunoglobulin • Surface IgG receptors are low in number and avidity • Therefore, immune complexes containing complement can bind to surface receptors on Raji Cells! • This can then help to detect immune complexes capable of binding complement • Sensitive test, however, warm reactive anti-lymphocyte antibodies and anti-ds-DNA antibodies may cause false positive results