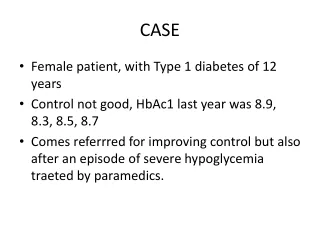
CASE
570 likes | 596 Vues
This case study focuses on a female patient with Type 1 diabetes who has suboptimal glycemic control and experienced a recent episode of severe hypoglycemia. The aim is to improve control and address the issues related to hypoglycemia.

CASE
E N D
Presentation Transcript
CASE • Female patient, with Type 1 diabetes of 12 years • Control not good, HbAc1 last year was 8.9, 8.3, 8.5, 8.7 • Comes referrred for improving control but also after an episode of severe hypoglycemia traeted by paramedics.
CASE • Patients states that se was relatively in good health until 2 years and since then her sugars are “out of wack”; she can go from the 400s to the lows 40s in a matter of hours and viceversa. Currently uses a combination of Lantus 34 units and Novolog (8, 9 and 10 units por BF, L and Supper). • Previous diagnosis include IBS with constipation and dyspepsia.
The Diabetic Stomach Jorge Calles-Escandon Director, Division of Endocrinology MetroHealth Regional Case Western Reserve University Cleveland, OH
Objectives 1. Review postprandial neuromuscular functions of the normal stomach 2. List gastric neuromuscular disorders of the diabetic stomach 3. Describe symptoms of and diagnostic approaches for diabetic gastroparesis 4. List diet, drug and device treatments for diabetic gastroparesis
Gastroparesis Gastro = stomach -paresis = weakness/paralysis Gastroparesis: A neuromuscular (motility) disorder of the stomach characterized by delayed gastric emptying without evidence of mechanical obstruction Term used in 1958 by Kassander as “gastroparesis diabeticorum” Kassander P.Ann Intern med 1958;48:797-812.
Gastroparesis in Patients with T1 and T2 Diabetes Mellitus ~2 million patients with T1 DM- 27 to 58% have gastroparesis ~20 million patients with T2 DM- 30 to 55% have gastroparesis ~6-7 million patients with DM have gastroparesis, many are undiagnosed, symptoms nonspecific, delay ranges from mild to severe Hasler WL. Current Gastro Reports 2007;9:261-269 Intagliato NI,Koch KL. Current Gastro Reports 2007;9:270-279
Normal postprandial gastric neuromuscular work: emptying a solid meal
Normal slow wave activity in body-antrum coordinates gastric peristalsisKLKoch, Sleisinger & Fortran, 2010
Slow waves + plateau/action potentials propagate from the pacemaker region through the body-antrum: gastric peristalsisKLKoch, Sleisinger & Fortran, 2010
Normal Gastric Neuromuscular Work requires normalSmooth muscle, Enteric neurons, interstitial cells of Cajal
Smooth Muscle, Enteric Neurons, Interstitial cells of Cajal (ICCs):Key elements of gastric neuromuscular work From Sanders et al. Handbook of Electrogastrography, 2007.
Gastric Work- mixing and emptying of a solid meal (technetium-labelled EggBeaters sandwhich-257 Calories)
Solid-phase Gastric Emptying:“Gastric output/work” over time[Normal output is >90% of solid meal (EggBeaters) emptied in 4hr]: Normal Delayed T=0 1 hr 2 hr 3 hr 4 hr
Gastric Neuromuscular Disorders (Gastropathies) in Diabetes Mellitusmodified from Koch Dig Dis Sci 1999;44:1061-1075.
Mechanisms underlying diabetic gastroparesis Vagal neuropathy Loss of gastric intrinsic inhibitory neurons Decreased numbers of interstitial cells of Cajal Acute hyperglycemia and chronic hyperglycemia (Results in gastric dysrhythmias, poor mixing/trituration, abnormal rates of emptying) Camilleri M. Diabetic Gastroparesis NEJM 2007;356:820-9.
Cellular Changes in Diabetic and Idiopathic Gastroparesis 40 Pts with gastroparesis (20 with DM, 20 Idiopathic) & 20 Controls Full thickness gastric body biopsies: Histological abnormalities were found in 83% of patients Defects in ICCs in 50% (cKit expression and cell ct) Abnormal immune infiltrate w. macrophages in 43% Loss of intrinsic neurons >idiopathic GP vs. DM *Decreased nNos >idiopathic (40%) vs. DM (20%) Increased connective tissue stroma Smooth muscle normal GpCRC. Farrugia et al. submitted for publication, 2010 * indicates finding is different in idiopathic and diabetic gastroparesis.
NIH Gastroparesis Consortitium NIH-funded Gastroparesis Clinical Research Centers Gastroparesis Registry– goal of 1000 patients with gastroparesis John Hopkins (J.Pasricha) California Pacific MC (W.Snape) Temple University (H.Parkman) University of Michigan (W.Hasler) University of Mississippi (T.Abell) University of Texas, El Paso (R.McCallum) Wake Forest University (K. Koch) MetroRegional (J. Calles, GLUMIT Ancillary) www.gcrgc.gov
Symptoms associated with Gastroparesis are related to ingestion of foodRevecki et al Aliment Pharmacol Ther 2003;18:141-50 • Nausea • Early Satiety • Prolonged fullness • Vomiting undigested food • Discomfort/pain in the epigastrium In DM: often T1 DM>10 yrs; poor/erratic glucose control & poor QOL Symptoms are non-specific and modestly associated with delayed rate of gastric emptying
Differential Diagnosis ofNausea and Vomiting 1.Mechanical Obstruction Pylorus, duodenum, small intestine, colon Hepatobiliary, pancreatic duct disease 2. Peptic Disease --- Any mucosal inflammation 3. Peritoneal irritation 4. Carcinoma Gastric, ovarian, hypernephroma, paraneoplastic synd.
Differential Diagnosis ofNausea and Vomiting 5. Metabolic/Endocrine DisordersDiabetic mellitus, Uremia, hypercalcemia Hypothyroidism, hyperthyroidism, Adrenal insufficiency, pregnancy 6. MedicationsChemotherapy agents, digitalis, cardiac anti-arrhythmic agents, NSAIDs, narcotics, nicotnine, progesterone, estrogen 7. Ischemic Gastroparesis--Chronic Mesenteric Ischemia 8. Postoperative Vagotomy with partial/total gastrectomy Fundoplication, Fundic resection
Differential Diagnosis of Nausea and Vomiting 9. Intestinal Pseudo-Obstruction Visceral neuropathy/myopathy, scleroderma, amyloidosis Idiopathic 10. CNS Disease Migraine, infections, tumors, complex partial seizures, vestibular nerve lesions, Parkinson’s disease 11. Psychological/Psychiatric Disorders Anorexia nervosa, bulimia nervosa, psychogenic nausea (vomiting) 12. Idiopathic Nausea and Vomiting with gastric dysrhythmia with gastroparesis (idiopathic, ?postviral) Cyclic vomiting syndrome
Patient Evaluation of Patient with N&V(and possible gastroparesis) Empiric Drug Trials (PPI, Prokinetic) Esophagitis Duodenitis Gastritis +H. pylori Endoscopy Mucosal evaulation Nausea and Vomiting of Unknown Origin Gastric Neuromuscular Dysfunction Gastric Neuromuscular Evaluation
Tests of Gastic Neuromuscular Function …beyond endoscopy… …beyond the gastric mucosa…
Solid-phase gastric emptying test: low fat EggBeaters meal over 4 hrs Tougas et al.Am J Gastro 2000;95:1456-1462
Solid-phase Gastric Emptying:“Gastric output/work” over time[Normal output is >90% of solid meal (EggBeaters) emptied in 4hr]: Normal Delayed T=0 1 hr 2 hr 3 hr 4 hr
Gastric Emptying, pH and contractions measured with the Capsule-Motility device (Smartpill)
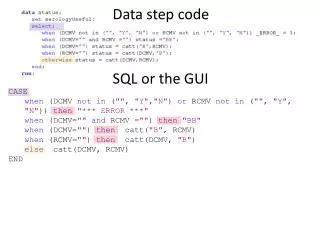
GI tract Transit Times measured by the Capsule Motility Device Controls Gastroparesis n=87n=60 GET* 3.6 hrs >5 hrs sbTT 5 hrs 5 hrs cTT 17 hrs 25 hrs *GET (gastric emptying time) EggBeaters meal SbTT (small bowel transit time); cTT (colonic transit time)
A Differential Diagnosis for Gastroparesis: Six causes/mechanisms Obstructive gastroparesis---Reversible Ischemic gastroparesis---Reversible Diabetic gastroparesis (type 1 and 2)---30% Postsurg. gastroparesis (BI/II antrectomy,fundoplica.)---20% Miscellaneous Causes (CVD, amyloid, muscular dystrophy) Idiopathic gastroparesis*---40% *(?postviral, ?drug-induced, ?degenerative or inflammatory processes--- injury to smooth muscle, enteric n., interstitial cells of Cajal, ANS)
Recording gastric myoelectrical activity (slow waves/action potentials) with surface electrodes: Electrogastrograms (EGGs)
Tachygastria in a Patient with Type 2 Diabetes Mellitus 60 sec. 500 µV Water Load 60 sec. 500 µV
Gastroparesis-Meals-Glucose/Insulin DyssynchonyHyper(hypo)glycemia
Treatment Approaches forDiabetic Gastroparesis Make the Diagnosis and provide Education: gastric dysrhythmias & gastroparesis Improve glucose control (<200 mg/dl) Reconsider standard ADA diet for patients with gastroparesis
Nausea and Vomiting (Gastroparesis) Diet Step 1: Gatorade and Bouillon--- hydration Small amt of liquids (Gatorade, To ingest 1000-1500 mL/d bouillon; salty with some caloriccontent) to avoid dehydration Multiple vitamin Step 2: Soups---Liquid nutrition Soup with noodles/rice To ingest 1500 calories/d Peanut butter, cheese, crackers to avoid dehydration and Caramels; chewy confections maintain weight 6 small-volume meals/d Multiple vitamin Step 3: Starches, Chicken, Fish---Solid nutrition Noodles, pastas, potatoes To find common foods that (mashed or baked), rice, baked are interesting and satisfying, chicken breast, fish and evoke minimal nausea 6 small-volume meals/d Multiple vitamin Diet Goal Avoid • Citrus drinks • Highly sweetened drinks • Creamy, milk-based liquids • Fatty foods • Red meats, fresh vegetables • Pulpy fibrous foods Adapted from Koch KL. Adv Gastroenterol Hepatol Clin Nutr. 1998;3:163-178.
Glucose Monitoring and Insulin Pump Therapy-Diabetic Gastroparesis (GLUMIT-DG): J. Calles/K. Koch & GpCRC
Treatment Approaches for Diabetic Gastroparesis Educate the patient: gastric dysrhythmias & gastroparesis Improve glucose control (<200 mg/dl) Drug therapy metoclopramide---CNS side effects (depression/tardive dyskin) erythromycin---causes N&V domperidone---not approved cisapride---withdrawn tegaserod---withdrawn BoTox injections(pylorus) ---? data ?ghrelin agonist --- in development Devices: G-tube for venting J-tube for enteral feeding Gastric electrical stimulation for refractory N&V Gastric Dysrhythmia and Gastroparesis (Severe Gastric Electro-Contractile Disorder)