Quick Guide
590 likes | 770 Vues
Quick Guide. For Clinicians Based on TIP 9 Assessment and Treatment of Patients With Coexisting Mental Illness and Alcohol and Other Drug Abuse. What is a TIP?.

Quick Guide
E N D
Presentation Transcript
Quick Guide For Clinicians Based on TIP 9Assessment and Treatment of Patients With Coexisting Mental Illness and Alcohol and Other Drug Abuse
What is a TIP? • The TIP series provides the substance abuse treatment and related fields with consensus-based, field-reviewed guidelines on substance abuse treatment topics of vital current interest. • This presentation is based on TIP 9 Assessment and Treatment of Patients With Coexisting Mental Illness and Alcohol and Other Drug Abuse (see last slide for ordering information). • For more detailed information, readers are referred by page number to the publication mentioned above.
Introduction • Treatment needs of patients who have a psychiatric disorder in combination with a substance abuse disorder differ significantly from the treatment needs of patient with either a substance abuse disorder or a psychiatric disorder by itself. • Clinicians must discriminate between psychiatry and substance abuse disorders by obtaining a thorough history of symptoms and disorders. See TIP 9, pp.1-3.
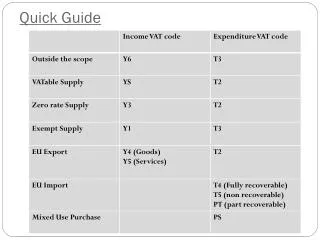
Dual Disorders Concepts and Definitions For more information, see TIP 9, pp.3-7.
Relationships: Substance Abuse and Psychiatric Symptoms and Disorders • Substance abuse may mask psychiatric symptoms, complicating the diagnostic process. • Terminology of dual disorders: • MICA: mentally ill chemical abusers • MISA: mentally ill substance abuser • CAMI: chemical abuse and mental illness • SAMI substance abuse and mental illness
Relationships • Patients with mental disorders have an increased risk for substance abuse disorders, and • Patients with substance abuse disorders have an increased risk for mental disorders.
Signs & Symptoms of Dependency/Addiction • Pathologic, often progressive and chronic process. • Compulsion and preoccupation with obtaining a drug or drugs. • Loss of control over use or substance abuse-induced behavior. • Continued use despite adverse consequences. • Tendency for relapse after period of abstinence. • Increased tolerance and characteristic withdrawal.
Components of Drug Dependence1 • Psychologic dependence: centers on the user’s need of a drug to reach a level of functioning or feeling or well-being. • Physical dependence: refers to the issues of physiologic dependence, establishment of tolerance, and evidence of an abstinence syndrome, or withdrawal upon cessation of substance abuse. 1 American Society of Addiction Medicine.
Symptoms: Substance Abuse • Significant impairment or distress resulting from use. • Failure to fulfill roles at work, home, or school. • Persistent use in physically hazardous situations. • Recurrent legal problems related to use. • Continued use despite interpersonal problems.
Medication Misuse • Describes the use of prescription medications outside of medical supervision or advice. • Not an abuse problem, it is a high-risk behavior. • May or may not involve or lead to substance abuse. • May promote the reemergence of psychiatric symptoms. • May cause toxic effects and psychiatric symptoms if it involved overdose.
Mental Health and Addiction Treatment Systems For more information, see TIP 9, pp.9-17.
Similarities of Mental Health and Addiction Treatment Systems • Variety of treatment settings and program types. • Public and private settings. • Multiple levels of care. • Biopsychosocial models. • Increasing use of case and care management.
Mental Health and Addiction Treatment Systems • Potential pitfall is prescribing psychoactive medications to psychiatric patient without first determining if the individual has a substance abuse disorder. • In treating dual disorders, a balance must be made between behavioral interventions and psychiatric medications as needed for the recovery process.
Treatment Models • Sequential: patient is treated by one system (addiction or mental health) and then by the other. • Parallel: simultaneous involvement of the patient in both mental health and addiction treatment settings. • Integrated: combines elements of both mental health and addiction treatment into a unified program for patients with dual disorders.
Critical Treatment Issues for Dual Disorder Treatment • Treatment engagement: initiating and sustaining patient’s participation. • Treatment continuity: between treatment programs and treatment components. • Comprehensiveness: includes collaborative integrated programs. • Treatment phases: detoxification, subacute stabilization, and long-term stabilization. • Continual reassessment and rediagnosis: involves collaboration across multiple systems.
Mood Disorders For more information, see TIP 9, pp.30-42.
Mood Disorders • Most common psychiatric diagnosis among patients with a substance abuse disorder. • More prevalent among patients using methadone and heroin. • Depression is common over the first months of sobriety whose symptoms may fade over time. • Mood disorder symptoms may be related to acute withdrawal symptoms from substances; adequate time should lapse prior to diagnosis of an independent mood disorder.
Substances That Precipitate or Mimic Mood Disorders • Depression and Dysthymia • During use (intoxication): alcohol, benzodiazepines, opioids, barbituates, cannabis, steroids (chronic), stimulants (chronic). • After use (withdrawal): alcohol, benzodiazepines, barbituates, opiates, steriods (chronic), stimulants (chronic).
Substances That Precipitate or Mimic Mood Disorders • Mania and Cyclothymia • During use (intoxication): stimulants, alcohol, hallucinogens, inhalants (organic solvents), steroids (chronic, acute). • After use (withdrawal): alcohol, benzodiazepines, barbituates, opiates, steroids (chronic).
Stages of Assessment • Assessing danger to self or others • Medical assessment • Initial addiction assessment • Social assessment • Violence towards others • Assessing mood symptomatology • Medical assessment • Psychiatric and addiction screening • Assessment instruments • Psychosocial assessment
Acute Treatment Strategies • Management of intoxication and withdrawal • Medical treatment • Psychiatric treatment
Subacute Treatment Issues • Matching patients and treatment • Psychiatric medications • Case management • Counseling and psychotherapy for depression • Levels of care • Family involvement in treatment settings • Professional and vocational planning • AIDS and HIV risk reduction
Long-Term Treatment Goals • Addiction treatment • Psychiatric treatment • Long-term treatment needs • Family issues • Eating disorders and gambling
Anxiety Disorders For more information, see TIP 9, pp.46-50.
Substance-Induced • Never assume anxiety symptoms or depersonalization are related to substance abuse. • Substance-induced conditions: • Panic • Phobias • Posttraumatic stress disorder • Obsessive-compulsive disorder
Anxiety • Most common symptom of people with substance abuse disorders. • Treatment of mild anxiety can be postponed to see if it resolves as addiction treatment progresses.
Long-Term Treatment • Medications are not a substitute for addiction treatment. • Cognitive-behavioral techniques are often as effective as medications, but generally take longer to achieve an equivalent response in the treatment of anxiety disorders. • For dual diagnosis patients, psychotherapy has significant advantages over substance abuse counseling alone, and can be incorporated into the substance abuse treatment.
Anxiety Treatment • Can be postponed unless anxiety interferes with substance abuse treatment. • Anxiety symptoms may resolve with abstinence and substance abuse treatment. • Affect-liberating therapies should be postponed until the patient is stable. • Psychotherapy, when required, should be recovery oriented.
Anxiety Treatment • Nonpsychoactive medications should be used when medications are needed. • Antianxiety treatments such as relaxation techniques can be used with and without medications. • A healthy diet, aerobic exercise, and avoiding caffeine can reduce anxiety.
Personality Disorders For more information, see TIP 9, pp.53-73.
Personality Disorders • Rigid, inflexible, and maladaptive behavior patterns of sufficient severity to cause significant impairment in functioning or internal stress. • If a personality disorder coexists with substance abuse, only the personality disorder will remain during abstinence. • Substance use often relates to the disorder to diminish symptoms, to enhance low self-esteem, to decrease feelings of guilt, and to amplify feelings of diminished individuality.
Most Challenging to Treat • Antisocial personality disorder, which involves a history of chronic antisocial behavior that begins before the age of 15 and continues into adulthood. • Borderline personality disorder, which is characterized by unstable mood and self-image, and unstable intense, interpersonal relationships. • Narcissistic personality disorder, which describes a pervasive pattern of grandiosity, lack of empathy, and hypersensitivity to evaluation by others. • Passive-aggressive personality disorder, which involves covertly hostile but dependent relationships.
Key Issues and Concerns • Patient contracting may involve a patient’s promise to avoid certain self-harm or high-risk behavior. • Transference and countertransference both rely on the mechanism of projection, a combination of personal past experiences along with feelings experienced during the course of therapy. • Clear boundaries are ethical and practical ground rules that help a therapist to be therapeutically helpful to patients.
Key Issues and Concerns • Changing roles of people with personality disorders may include: the victim, the persecutor, and the rescuer. • Resistance involves patients with personality disorders who often exhibit acting-out behaviors that were developed as psychological defenses and survival techniques. • Subacute withdrawal may include mood swings, irritability, impairment in cognitive functioning, short- and long-term memory problems, and intense craving for substances.
Key Issues and Concerns • Symptom substitutions are compulsive behaviors that includes eating disorders, compulsive spending, gambling, and sex. • Somatic complaints: therapists should watch for use of prescription and over-the-counter drugs and for drug-seeking behaviors. • Therapist well-being can be compromised when working with patients with personality disorders. Therapists should join or develop support systems with others in the field.
Borderline Personality Disorder • Therapist should engage patient by acknowledging/joining the patient’s need for safety. • Assessment should include: history of substance abuse and mental health treatment, suicidal planning, dissociative experiences, psychosocial history, history of sexual abuse, and a history of psychotic thinking. Could require a neurological examination. • Avoid psychodynamic confrontations with patient. • Long-term care may include individual counseling, group therapy, 12-step participation, and the continuum of care.
Antisocial Personality • In engaging the patient, it is useful to join with the patient’s world view. • Assessment should include a thorough family history, including a sexual history that includes questions about animals and objects. Other topics should be bonding, parasitic relationships, head injuries, fighting, and being hit. • Avoid angry confrontations since patients may engage in dangerous physical behavior to avoid unpleasant situations or activities. • Long-term care includes individual counseling, group therapy, and the continuum of care.
Narcissistic Personality Disorder • To engage, therapeutically address patient traits such as hypersensitivity, need for control, rage, and depression. • Assessment should include survival skills/self-care, monitor use of OTC drugs, treatment provider history, psychosocial and substance abuse history, medication evaluations for antidepressants, and identification of typical passive-aggressive maneuvers of patient. • Several issues, such as responses to abusive relationships, obtaining safe housing, and receiving emergency psychiatric admissions for suicidal crises must be managed by the therapist. • Long-term care may include individual counseling, group therapy, 12-step participation, and the continuum of care.
Coordination of Care • Maintaining ongoing contacts is essential for all patients with personality disorders. • Issues to remember in coordination of care: • Primary case manager • Legal issues • Managed care • Funding issues • Staffing and cross-training • Medical issues • Integration into 12-step self-help groups
Psychotic Disorders For more information, see TIP 9, pp.76-85.
Psychotic Disorders • Stimulant-Induced Symptoms • Acute stimulant intoxication (chronic) can cause symptoms of psychosis. Included are: delirium, delusions, prominent hallucinations, incoherence, and loosening of associations. Stimulant delirium often includes formication (a tactile hallucination of bugs crawling on or under the skin). • Depressant-Induced Symptoms • Acute withdrawal from alcohol, barbiturates, and benzodiazepines can produce a withdrawal delirium, especially with heavy use and high tolerance due to a concomitant physical illness. • Psychedelic- and Hallucinogen-Induced Symptoms • Psychotic symptoms are possible in chronic, high-dose patterns due to virtue of drugs’ stimulant properties. Can cause hallucinogenic hallucinosis, characterized by perceptual distortions, maladaptive behavioral changes and impaired judgment.
Engaging the Chronically Psychotic Patient • Noncoercive Engagement Techniques • Assistance obtaining food, shelter, and clothing • Assistance obtaining entitlements and social services • Drop-in centers as entry to treatment • Recreational activities • Low-stress, nonconfrontational approaches • Outreach to patient’s community • Coercive Engagement Techniques • Involuntary commitment • Mandated medications • Representative payee strategies
Pharmacological Management For more information, see TIP 9, pp.91-97.
Pharmacologic effects • Therapeutic effects include indicated purposes and desired outcomes such as a decrease in the frequency and severity of episodes of depression produced by antidepressants. • Detrimental effects include unwanted side effects, such as dry mouth or constipation resulting from antidepressant use.
Dual Disorder Patients • Special attention should be given to detrimental effects, in terms of: • Medication compliance • Abuse and addiction potential • Substance abuse disorder relapse • Psychiatric disorder relapse
Pharmacologic Risk Factors • Psychoactive Potential • Not all psychiatric medications are psychoactive. • Psychoactive medications can cause acute psychomotor effects and a relatively rapid change in mood or thought. • Reinforcement Potential • Some drugs promote reinforcement or increased likelihood of repeated use. • Can occur by either the removal of negative symptoms or conditions, or the amplification of positive symptoms or states. • Involves strengthening that a certain behavior will be repeated for reward and satisfaction, as with drug-induced euphoria. • Tolerance and Withdrawal Potential • Long-term or chronic use can cause tolerance to therapeutic effects and dosage increases to recreate desired effects. • Drugs that promote tolerance and withdrawal generally have higher risks for abuse and addiction.
Prescribing Medication • High-risk patients should include a benefit analysis that considers: • The risk of medication abuse. • The risk of undertreating a psychiatric problem. • The type and severity of the psychiatric problem. • The relationship between the psychiatric disorder and the substance abuse disorder for the individual patient. • The therapeutic benefits of resolving the psychiatric and substance abuse problems.
Psychotherapy Cognitive therapy Behavioral therapy Relaxation skills Meditation Biofeedback Acupuncture Hypnotherapy Self-help groups Support groups exercise Education Nonpharmacologic Approaches
Antihistamines • Frequently prescribed for mild anxiety and insomnia. • Exert mild anxiolytic and hypnotic effects, lack euphoric properties, and do not promote physical dependence. • High doses can cause acute delirium, alter mood, or cause morning-after depression. • Patients in recovery should be discouraged from purchasing and using OTC antihistamines.
Antidepressants • Effective for treatment of depression, anxiety disorders, including generalized anxiety disorder, phobias, and panic disorder. • They are not euphorigenic and do not cause acute mood alterations. • Some exert a mild sedating effect, while others exert a mild stimulating effect. • Anticholinergic effects include: dry mouth, blurred vision, constipation, urinary hesitancy, and toxic-confusional states. • Adrenergic activation symptoms may include: tremor, excitement, palpitation, orthostatic hypotension, and weight gain.