Central Venous Catheterization
E N D
Presentation Transcript
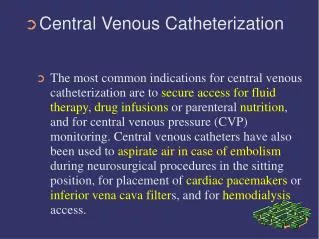
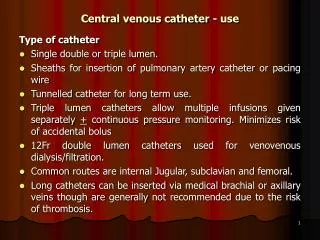
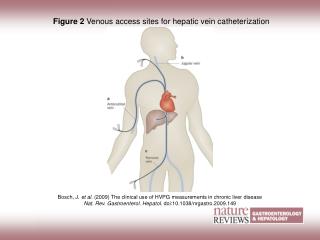
Central Venous Catheterization The most common indications for central venous catheterization are to secure access for fluid therapy, drug infusions or parenteral nutrition, and for central venous pressure (CVP) monitoring. Central venous catheters have also been used to aspirate air in case of embolism during neurosurgical procedures in the sitting position, for placement of cardiac pacemakers or inferior vena cava filters, and for hemodialysis access.
Central Venous Catheterization While central venous lines are placed primarily for venous access, useful information occasionally can be obtained by measuring the CVP. The CVP may be useful in a hypotensive trauma patient to differentiate pericardial tamponade from hypovolemia. Pericardial tamponade causes elevation and equalization of the right atrial, pulmonary artery diastolic and wedge pressures.
Central Venous Catheterization Analysis of the CVP tracing may also be helpful in the diagnosis of pericardial tamponade (y descent is damped or absent due to restricted early ventricular filling), tricuspid insufficiency (v wave becomes prominent, the x descent is obliterated and the y descent is steep), and in the differential diagnosis of certain cardiac arrhythmias (i.e., a wave is absent in patients with atrial fibrillation, and flutter a waves at a regular rate of 250 to 300 per minute frequently are observed in patients with atrial flutter).
Central Venous Catheterization A properly placed catheter can be used to measure right atrial pressure which, in the absence of tricuspid valve disease, will reflect the right ventricular end-diastolic pressure. A central venous pressure (CVP) catheter can not be used to assess left ventricular function in critically ill patients, since ventricular disparity and independence of right and left atrial pressures have been confirmed repeatedly in these patients.
Massive Hemothorax Incidence of haemothorax and haemopneumothorax ~50-60% in penetrating trauma 60-70% in blunt trauma. Majority are not massive Massive haemothorax defined as >1500 ml of blood in chest cavity
Massive Hemothorax Clinical Signs: Unilateral dullness to percussion Shock Unilateral absence of breath sounds Deviation of trachea Neck veins may be flat due to severe hypovolaemia or distended because of the mechanical effects of intrathoracic blood Blood loss complicated by hypoxia
Massive Hemothorax Management manage initially by simultaneous restoration of volume deficits and decompression of chest cavity. If auto-transfusion device is available it should be used emergency thoracotomy for massive haemothorax or haemothorax with ongoing loss of >200 ml of blood per hour for 3-4 h
Emergency Thoracotomy Indications:patients who have sustained truncal trauma and remains unstable or moribund despite adequate resuscitation by way of infusion, chest drainage and ventilation Lack of pupillary response is not a contraindication to operation, though it is an indication for thoracotomy in casaulty rather than transfer to theatre Patients who have shown no respiratory effort and no cardiac output since pick-up will not survive
Emergency Thoracotomy Criteria for discontinuation of resuscitation: Irretrievable anatomic injury (eg ruptured heart) Failure of volume resuscitation within 15 mins of starting Failure to sustain spontaneous cardiac rhythm and maintain mean systemic blood pressure > 50 mmHg, with or without inotropic support, within 30 mins
Emergency Thoracotomy In general those who survive with reasonable cerebral function are young, previously fit and have only a short period of circulatory arrest Patients with blunt trauma have a poor outcome and it may be deemed unwise even to consider further measures if standard resuscitation fails Overall only 5% of those undergoing emergency thoracotomy survive and many of these have prolonged convalescence and cerebral damage
Urgent surgery Purpose is to repair structures that will not heal optimally without surgery and to prevent late complications
Urgent surgery- Absolute indications Cardiac arrest due to tamponade or exsanguination Significant and continued haemorrhage: immediate blood loss > 1500 ml; Loss > 500 ml in first hr. or 200 ml/hr thereafter Decision to operate should be made early before occurrence of a dilutional coagulopathy Dangerous predicted track/mediastinal traversing Massive air leak Certain specific injuries
Urgent surgery- Relative indications: Thoracoabdominal injury Bullet embolism High-velocity gunshot wound Missile retrieval. In general missiles should only be removed if they pose a risk of embolization from heart or pulmonary artery, erosion of adjacent structures due to repetitive cardiorespiratory movements or infection due to non-metallic pieces Certain specific injuries
Urgent surgery- Relative contraindications: Cardiac contusion Pulmonary parenchymal contusion Pneumomediastinum (without other injury). Exclude tracheobronchial tear, pneumothorax, oesophageal perforation or gas forming organisms within pericardium
Priorities with multiple injuries Thoracic hemorrhage or tamponade Abdominal hemorrhage Pelvic hemorrhage Extremity hemorrhage Intracranial injury Acute spinal cord injury
Second-priority Injuries for Surgical Treatment after Resuscitation
Clinical analysis of craniocerebral trauma complicated with thoracoabdominal injuries in 2165 cases. Chinese journal of traumatology2004 Jun;7(3):184-7.Chen WQ, Wang G, Zhao W, He LZ. July 1993 - June 2003 382 severe craniocerebral trauma (167 with shock), 733 thoracic injuries, 645 abdominal injuries and 787 thoraco-abdominal injuries. 294 developed shock on admittance
Craniocerebral Trauma Complicated with Thoracoabdominal Injuries Traditional views:Hypotension in traumatic shock should be treated with fluid resuscitation with vaso-active substances to raise blood pressure. New concepts:Delayed resuscitation
Craniocerebral Trauma Complicated with Thoracoabdominal Injuries Delayed resuscitation Suggested for shock caused by pure active hemorrhage without complicated CCT or ↑ICP Small volume of balanced saline to satisfy the body`s basic needs instead of rapid large volumes of fluid resuscitation for patients present with active hemorrhage. In patients with severe CCT, early resuscitation with a large volume of fluid would aggravate cerebral edema.
Craniocerebral Trauma Complicated with Thoracoabdominal Injuries For intracranial hematoma with serious thoracic / abdominal hemorrhage and need hemostasis, fluid transfusion should be appropriately controlled (SBP, 90 mm Hg) Prevent ischemia and hypoxia in important organs, and aggravation of hemorrhage Prompt hypertonic and hyperosmotic solution and whole blood to ensure fast restoration of BP and improvement in microcirculation and to reduce the volume of solution to be infused
Craniocerebral Trauma Complicated with Thoracoabdominal Injuries Hypertensive drugs Should not be administrated for mild shock Small quantity is suggested for moderate shock For severe shock, should be given at early stage to improve the diseased condition for fluid infusion against shock. Those who need continuous support from hypertensive drugs probably have poor prognosis. Tend to develop multiple organ dysfunction syndrome (MODS) at advanced stage.
Craniocerebral Trauma Complicated with Thoracoabdominal Injuries Since complicated thoracic trauma is more complex than pure craniocerebral trauma, in the present study, firstly dealt with low blood pressure caused by thoracic trauma Unblocking the respiratory tract Relieving compressed lungs Restricting abnormal thoracic activities
Craniocerebral Trauma Complicated with Thoracoabdominal Injuries Life-saving operation Cerebral hernia(-) hemorrhagic shock(-) Craniotomy first when cranial hematoma was large, and laparotomy and/or thoracotomy first when rapid hemorrhage was present Hernia of brain(+) hemorrhagic shock(-) Craniotomy first and then thoracotomy Hemorrhagic shock (+) cranial hernia(-) Thoracotomy or laparotomy first and then craniotomy Both intracranial hematocele and severe hemorrhagic shock Craniotomy and thoracotomy or laparotomy at the same time.
Craniocerebral Trauma Complicated with Thoracoabdominal Injuries Brain-stem failure vs Severe shock Shock, deep coma, bilateral pupil dilation, irregular breathing Severe shock Large volumes of uncoagulated blood could be drained Symptoms improved.after antishock treatment Patients who need large doses of hypertensive drugs or great amount of fluid transfusion Thoracotomy or laparotomy first to achieve hemostasis. Measures which do not aggravate disturbance in respiratory and circulatory systems are recommended as early as possible