GASTROINTESTINAL BLEEDING
330 likes | 2.02k Vues
GASTROINTESTINAL BLEEDING . Acute upper gastrointestinal bleeding Haematemesis : is the vomiting of blood from a lesion proximal to the distal duodenum.

GASTROINTESTINAL BLEEDING
E N D
Presentation Transcript
Acute upper gastrointestinal bleeding Haematemesis : is the vomiting of blood from a lesion proximal to the distal duodenum. • Melaena is the passage of black tarry stools; the black colour is due to blood altered by bacteria - 50 mL or more is required to produce this. • Melaena can occur with bleeding from any lesion from areas proximal to and including the caecum. • Following a massive bleed from the upper GI tract, unaltered blood (owing to rapid transit) can appear per rectum, but this is rare. • The colour of the blood appearing per rectum is dependent not only on the site of bleeding but also on the time of transit through the gut.
The causes for upper GI hemorrhage include the following: • Esophageal causes: • Esophageal varices • Esophagitis • Esophageal cancer • Esophageal ulcers • Gastric causes: • Gastric ulcer • Gastric cancer • Gastritis • Gastric varices • Gastric antral vascular ectasia. • Duodenal causes: • Duodenal ulcer • Vascular malformations. • Hematobilia, or bleeding from the biliary tree • Hemosuccuspancreaticus, or bleeding from the pancreatic duct
Peptic ulceration is the commonest cause of serious and life threatening gastrointestinal bleeding. • Drugs. Aspirin (even 75 mg a day) and other NSAIDs can produce gastric lesions. • These agents are also responsible for GI haemorrhage from both duodenal and gastric ulcers, particularly in the elderly. Corticosteroids in the usual therapeutic doses probably have no influence on GI haemorrhage. • Anticoagulants do not cause acute GI haemorrhage per se but bleeding from any cause is greater if the patient is anticoagulated.
The following factors affect the management: • age • the amount of blood lost, which may give some guide to the severity • continuing visible blood loss • signs of chronic liver disease on examination • evidence of co-morbidity, e.g. cardiac failure, ischaemic heart disease, renal disease and malignant disease • presence of the classical clinical features of shock (pallor, cold nose, tachycardia and low blood pressure ) • With liver disease, the bleeding is often severe and recurrent if it is from varices. Splenomegaly suggests portal hypertension but its absence does not rule out oesophagealvarices. • With shock, remember that the peripheral arterial constriction that occurs may keep the blood pressure falsely high.
Management of acute gastrointestinal bleeding • Rapid history and examination. • Monitor the pulse and blood pressure half-hourly. • Take blood for haemoglobin, urea, electrolytes, ,liver functions ,blood grouping and crossmatching . • Establish intravenous access - central line if brisk bleed. • Give blood transfusion/colloid if necessary. • Stop drugs, e.g. NSAIDs, warfarin • Indications for blood transfusion are: • (a) SHOCK (pallor, cold nose, systolic PB below 100 mmHg, pulse > 100 b.p.m.) • (b) haemoglobin < 10 g/dL in patients with recent or active bleeding. • Oxygen therapy for shocked patients. • Urgent endoscopy in shocked patients/liver disease. • Continue to monitor pulse and BP. • Re-endoscope for continued bleeding/hypovolaemia. • Surgery if bleeding persists.
Urgent resuscitation is required in patients with large bleeds and the clinical signs of shock. • Oxygen should be given by face mask and the patient should be kept nil by mouth until endoscopy has been performed. • The major principle is to rapidly restore the blood volume to normal. This can be best achieved by transfusion of whole blood via one or more large-bore intravenous cannulae; physiological saline is given until the blood becomes available . • The rate of blood transfusion must be monitored carefully to avoid overtransfusion and consequent heart failure. • The pulse rate and venous pressure are the best guides to transfusion rates.
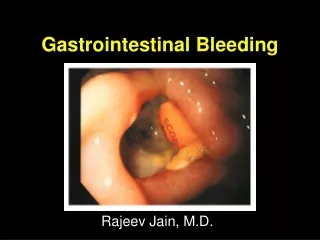
Endoscopy • should be performed within 24 hours in most patients. Early endoscopy helps to make a diagnosis and to make decisions regarding discharge from hospital, particularly in patients with minor bleeds and under 60 years of age. • Urgent endoscopy (i.e. after resuscitation) should be performed in patients with shock, suspected liver disease or with continued bleeding. • Endoscopy can detect the cause of the haemorrhage in 80% or more of cases. In patients with a peptic ulcer, if the stigmata of a recent bleed are seen (i.e. a spurting artery, active oozing, fresh or organized blood clot or black spots) the patient is more likely to re-bleed.
At first endoscopy: varices should be injected. • all bleeding ulcers should be either injected with epinephrine (adrenaline), the vessel coagulated either with a heater probe or with laser therapy or metallic clips applied. • These methods reduce the incidence of re-bleeding, although they do not significantly improve mortality as re-bleeding still occurs in 20% within 72 hours. • Intravenous omeprazole 80 mg followed by infusion 8 mg/h for 72 hours should be given to all patients in this group, as it reduces re-bleeding rates and the need for surgery. • Drug therapy :There is little evidence that H2-receptor antagonists or proton-pump inhibitors (PPIs) affect the mortality rate of GI haemorrhage, but PPIs are usually given to all patients with ulcers because of their longer-term benefits. • Somatostatin (which reduces the splanchnic blood flow as well as acid secretion) can be given as an infusion if the bleeding is difficult to stop.
Risk factors • Age is clearly significant. Below the age of 60 years mortality from GI bleeding is small, < 0.1%, but above the age of 80 the mortality is greater than 20%. • Patients with recurrent haemorrhage have an increased mortality. • Most re-bleeds (approximately 20% of all cases) occur within 48 hours. • Co-morbidity invariably increases mortality. • Presence of shock at any time increases mortality.
Lower GIT bleeding • Acute lower gastrointestinal bleeding • Massive bleeding from the lower GI tract is rare. • On the other hand, small bleeds from haemorrhoids occur very commonly. • Massive bleeding is usually due to diverticular disease or ischaemic colitis.
The causes of lower gastrointestinal bleeding are • Coagulopathy - specifically a bleeding diathesis • Colitis • ischaemic colitis • ulcerative colitis • infectious colitis • E. coli . • Shigella • C. difficile • Campylobacter jejuni • Hemorrhoids • Angiodysplasia • Neoplasm - cancer • Diverticular disease - diverticulosis, diverticulitis
Most acute lower GI bleeds start spontaneously. The few patients that continue bleeding and are haemodynamically unstable need resuscitation using the same principles as for upper GI bleeding . Surgery is rarely required. • A diagnosis is made using the history, and the following investigations as appropriate: rectal examination (e.g. carcinoma) • proctoscopy (e.g. anorectal disease, particularly haemorrhoids) • sigmoidoscopy (e.g. inflammatory bowel disease) • barium enema - ischaemic colitis • colonoscopy - for any mucosal lesion and removal of polyps • angiography - vascular abnormality (e.g. angiodysplasia ) • Isolated episodes of rectal bleeding in the young (< 45 years) only require rectal examination and sigmoidoscopy. Colorectal cancer is rare in this age group without a strong family history. Individual lesions are treated as appropriate.
Chronic gastrointestinal bleeding • Patients with chronic bleeding usually present with iron-deficiency anaemia . • Chronic blood loss producing iron deficiency anaemia in all men and all women after the menopause is always due to bleeding from the gastrointestinal tract, often from a right-sided colonic neoplasm which must be excluded. Occult blood tests are necessary .
Measurement of faecal occult blood • It is only of value in: premenopausal women - if a history of menorrhagia is uncertain and the cause of iron deficiency is unclear • mass population screening for large bowel malignancy. • Advantages: cheap and easy to perform. • Disadvantages: high false-positive rate, leading to unnecessary investigations
Diagnosis • Chronic blood loss can occur with any lesion of the gastrointestinal tract that produces acute bleeding . • It is, however, usual for oesophagealvarices to bleed severely and rarely to present as chronic blood loss. • It should be remembered that, world-wide, hookworm is the most common cause of chronic gastrointestinal blood loss. • History and examination may indicate the most likely site of the bleeding, but if no clue is available it is usual to investigate both the upper and lower gastrointestinal tract endoscopically at the same session ('top and tail'). • For practical reasons an upper gastrointestinal endoscopy is performed first as this takes only minutes, followed by colonoscopy when any lesion can be removed or biopsied. • A barium enema is performed only if colonoscopy is unavailable. A small bowel follow-through is the next investigation, but the diagnostic yield is very low
Endoscopes to visualize the whole of the small bowel (enteroscopy) are available at specialist centres. • Wireless capsule endoscopy is useful, particularly with melaena of obscure origin (90% of causes were found in a recent study). • Treatment :The cause of the bleeding should be treated, if found. Oral iron is given to treat anaemia