Eating Disorders
630 likes | 825 Vues
Eating Disorders. Joan R. Griffith, MD, MHA, MPH Associate Professor Department of Pediatrics University of Toledo. Objectives. Review eating disorders categories Discuss salient research studies. Case Presentation.

Eating Disorders
E N D
Presentation Transcript
Eating Disorders Joan R. Griffith, MD, MHA, MPH Associate Professor Department of Pediatrics University of Toledo
Objectives • Review eating disorders categories • Discuss salient research studies
Case Presentation • 15 yo female with history restricted food intake and poor weight gain over past 6-9 months • Active in school, friends have noticed her decreased food intake • Significant family dynamics • BMI 16
Introduction 1 • “Understanding the complexities of eating disorders, such as influencing factors, comorbid illness, medical and psychological complications, and boundary issues, is critical in the effective treatment of eating disorders” -- American Dietetic Association Position Statement, J Am Diet Assoc.2006 Dec;106(12):2073-2082
Introduction 2 • News media’s role in shaping public perception of eating disorders -- Simplifies and sensationalizes versus view as complex medical phenomena -- Impact on insurance coverage: “serious or biologically based” -- Stigma: “fear, hostility, disapproval versus compassion, support, understanding” -- O’Hara & Smith. Patient Education and Counseling.2007;68:43-51
Introduction 3 • British polls: -- 35% feel patients should “pull themselves together” -- 33% blame the individual --- View AN as “extreme form of dieting, often for narcissistic motives” • 2005 National Eating Disorders Association sponsored poll of American adults for primary causes of eating disorders: -- Dieting (66%) -- Media (64%) -- Families (52%) -- Genetics (33%) -- O’Hara & Smith. Patient Education and Counseling.2007;68:43-51
Dieting Data • Prevalence of eating disorders in teens increased during past 50 years • 40% to 60% of high school girls in US diet to lose weight • 13% induce vomiting or use diet pills, laxatives or diuretics • 30% - 40% of junior high girls admit concern about weight
Eating Disorder Categories • Anorexia nervosa (AN) • Bulimia nervosa (BN) • Eat disorder not otherwise specified (EDNOS) • Binge-eating disorder (rarely seen in adolescents)
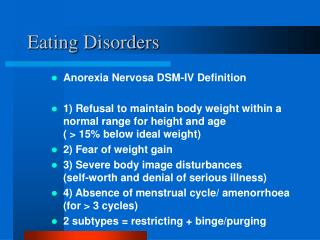
Anorexia Nervosa:Diagnostic and Statistical Manual of Mental Disorders (DSM) IV Criteria • Refusal to maintain body weight at or above minimally normal for age & height • Intense fear of gaining weight or becoming fat, even though underweight • Disturbance in the way in which one’s body weight or shape is experienced, or shape on self evaluation, or denial of the seriousness of the current low weight
DSM IV Criteria--continued • In post-menarcheal females, amenorrhea, i.e., absence of at least 3 consecutive menstrual cycles • Type: a. Restricting type b. Binge-eating/purging type
Anorexia Nervosa • 90% to 95% are females • 90% diagnosed before age 25 years • Two peaks for symptoms begin: - 13 to 14 years - 17 to 18 years • Diagnosis may be delayed 1 to 2 years
Anorexia Nervosa • Prevalence in US and Great Britain: 0.5% of adolescent females • Middle & upper socioeconomic classes - 1 in 300 of 15-19 yr girls in elite private schools • Increasing in other ethnic/racial groups and SES
Etiology/Pathogenesis • Biologic/genetic evidence -- Biomedical framework: genetic and environmental* -- Genetic factors explain more than 50% of risk for developing eating disorder* • Increased in monozygotic twins • Increased incidence in sisters • Increased prevalence of affective disorders in families
Psychological • Personality traits: negative emotionality, perfectionism, drive for thinness, poor interoceptive awareness, ineffectiveness, obsessive-compulsive* • Family characteristics: enmeshment, over-protectiveness, rigidity, lack of conflict resolution and history of early separation stress and sexual abuse -- Lilenfeld et al. Clinical Psychology Review.2006;26:299-230.
Socio-cultural stressors • Affluence in industrial countries • Social standard: thinness = beauty • Media bombardment: thinness = success • Media: women as sex objects • Some sport requirements for thinness: gymnastics, distance running & ballet
Presenting Symptoms • Excessive weight loss -- Female: 100 lbs at 5 feet plus 5 lbs for each additional inch -- Male: 106 lbs at 5 feet plus 5 lbs for each additional inch • Primary or secondary amenorrhea • GI symptoms: abdominal pain, vomiting, or bloating • Growth failure or pubertal delay
Differential Diagnosis • Thyroid disease • Diabetes mellitus • Addison disease • Inflammatory bowel disease • Brain tumors • Malignancy • HIV
DDx--continued • Drug/alcohol abuse • Depression • Schizophrenia • Personality disorders • Obsessive/compulsive disorders
Diagnosis: Detailed History • Weight • Diet • Exercise • Body image • Self-induced binging; purging • Self-medication with laxatives, diuretics, or diet pills
Diagnosis— Detailed Hx continued • Menstrual/puberty • Sexual/physical abuse history • Family history of psychiatric illness, alcoholism, and eating disorders • Substance abuse, sexual behaviors, compulsive/impulsive behaviors
Physical Exam • Significant weight loss or failure to make expected gain • Bradycardia, hypotension, orthostatic hypotension, hypothermia • Acrocyanosis, edema, cool mottled discoloration of extremities • Skin: lanugo, loss of scalp hair, jaundice, dry skin
Physical Exam--continued • Musculoskeletal weakness, loss of muscle mass • Cardiac arrhythmias
Lab Findings Results of following are usually normal: • CBC: rare to find anemia • Lytes: unless associated with vomiting • BUN: low to normal even with dehydration • LFTs: increased with severe starvation due to fatty liver
Labs--continued Results of following sometimes abnormal • UA: alkaline with ketones and protein • Cholesterol: elevated • Amylase: elevated • ECG: bradycardia, low voltage & nonspecific ST and T wave changes, prolonged QT • Bone densitometry: may show osteopenia
Labs--continued • Results usually abnormal • LH & FSH: low • TFTs: low • Cortisol: high
Treatment Role of Primary Care Provider (PCP) • Diagnosing the eating disorder • Setting weight goals • Planning with patient how to meet goal • Negotiating consequences if goal not met • Makes referrals and coordinates care: psychotherapist, nutritionist
Treatment--continued • Manages complications of the eating disorder • Provides care for inter-current illnesses • Establishes clear criteria for hospitalization if treatment started as outpatient
Treatment--continued • Outline plans for changing unhealthy behaviors, e.g., binging, vomiting, dieting, excessive exercise
Psychotherapy Close relationship with PCP • Individual, family and/or group therapy • Antidepressants as needed
Nutrition • Patient & family education • Weight gain goal of 1 pound per week for outpatient and 3 pounds per week for inpatient • Normal active female adolescent requires about 1500 kcal/day to maintain weight; -- AN may consume only 600 to 1000 kcal/day • AN patients may require 2000 – 3000 calories/day for sustained weight gain as 3 meals and 2-4 snacks per day
Indications for Hospitalization 1 Physiologic • Weight 30% or more below ideal body weight • Severe metabolic/cardiovascular problems • Unusual presentation
Indications for Hospitalization 2 Psychiatric • Severe depression or suicide risk • Acute psychosis • Uncontrollable binging & purging • Acute food refusal • Severe family dysfunction or family crisis
Outcome • 50% of patients recover fully • 30% recover partially, i.e., continue to have dysfunctional eating, body image distortion, and impaired social relationships but do well in school/job • Approximately 20% remain chronically ill • AN has the highest rate of mortality of any psychiatric disorder* -- O’Hara & Smith. Patient Education and Counseling.2007;68:43-51. *-- Franko & Keel. Clinical Psychology Review.2006;26:769-782.
Refeeding Syndrome • Severely malnourished patients (at least 30% below average body weight for height) • Risk of developing severe complications if refed too rapidly: -- Edema -- Fatty liver -- Hypophosphatemia --- Cardiac failure, CNS depression, hemolytic anemia • Can occur with oral, enteral or parental feeding • Prevention: use prophylactic phosphorus and refeed slowly (800-1000 calories/day and increase by 100-200 calories/day) -- C Holland-Hall & RT Brown. Adolescent Medicine Secrets.2002. Hanley & Belfus, Inc, Philadelphia.
Case Presentation • 15 yo female with history of recurrent vomiting and diarrhea since Feb 2007 • Weight in 90th percentile for age and height • PE: Flat affect, marked erosion of dental enamel • 10-26-08: admitted for full work-up including GI evaluation; WNL • 10-30-08: Psychology referral. Mother asks, “Does she look like she has an eating disorder?”
Bulimia Nervosa • College age: 1% to 5% women; 1% men • Secondary school: 1.1% girls; 0.2% boys • Incidence is increasing • Partial syndrome of vomiting and/or laxative use without binge-eating may be more common, especially in college students • Do not have adequate knowledge of the etiology & maintenance of the syndrome
DSM-IV Diagnostic Criteria • Recurrent episodes of binge eating -- Binge characterized by both: 1. Eating in a discrete period of time, an amount of food larger than most people would eat during a similar period of time & under similar circumstances 2. A sense of lack of control over eating
DSM-IV Continued • Recurrent inappropriate compensatorybehavior to prevent weight gain, e.g., self-induced vomiting, laxatives, diuretics, enemas, fasting, excessive exercise • Binging and inappropriate compensatory behaviors both occur at least twice a week for 3 months
DSM-IV Continued • Self evaluation is unduly influenced by body shape and weight • The disturbance does not occur exclusively during episodes of anorexia nervosa • 2 Types: -- Purging -- Non-purging
Etiology & Pathogenesis • Biologic factors: 1. Dysregulation of serotonin metabolism resulting in binge eating of high-carbohydrate foods 2. Family history of alcoholism and affective disorders, e.g. depression
Etiology Continued • Psychological factors: 1. History of incest, rape or sexual abuse 2. Dysfunctional family interactions -- parental enmeshment to absence -- chaotic, conflicted & critical • Lead to feelings of being out of control, poor self-esteem, and needing comfort
Etiology-- Psychological Continued • Personality differences in AN and BN -- AN: anxious, inhibited, controlled -- BN: affectively labile, under controlled, active
Etiology Continued • Socio-cultural factors: 1. Strong pressures for thinness lead to dissatisfaction with normal or overweight -- physically attractive/socially acceptable 2. May begin after unsuccessful dieting 3. “Contagion” factors in college dorms for binging and purging “parties”
Differential Diagnosis • Thyroid disease • Diabetes mellitus • Addison disease • Inflammatory bowel disease • Brain tumors • Malignancy • HIV
DDX Continued • Drug/alcohol abuse • Depression • Schizophrenia • Personality disorders • Obsessive/compulsive disorders
Diagnosis--History • Weight history • Detailed diet history • Detailed exercise history • Body image history • History of self-induced binging; purging; self-medication with laxatives, diuretics, or diet pills
Diagnosis--HX Continued • Detailed menstrual/puberty history • Sexual/physical abuse history • Family history of psychiatric illness, alcoholism, and eating disorders • History of substance abuse, sexual behaviors, compulsive/impulsive behaviors
Physical Examination • Head & neck: bilateral parotid gland swelling, loss of tooth enamel (from acidic stomach contents), dental caries, subconjunctival hemorrhage (from forced vomiting) • Skin: scarring or hyperpigmentated calluses on knuckles (Russell’s sign); petechiae on face (from forced vomiting)
Physical Exam Continued • GI: abdominal distention, ileus, constipation, rectal bleeding, gastritis, esophagitis, esophageal tears • Pulmonary: aspiration pneumonia, pneumomediastinum • Cardiac: arrhythmias
Outcome • Variable course; majority chronic fluctuation of binge/purge behavior • Pts with history of sexual abuse, conflicting family environments, comorbid medical or psychiatric states, or inability to seek or accept Rx have more severe course • BN tend to be more responsive than AN -- 60% BN vs. 50% AN recover in first 5 years